
Primary thrombophilia XV: antithrombotic treatment of sticky platelet syndrome worldwide
Introduction
The condition known as sticky platelet syndrome (SPS) was first described in 1983; however, its prevalence did not receive substantial recognition in medical literature until much later (1-25). SPS is a relatively common cause of thrombosis (20,26-31), and is associated with both unexplained arterial and venous thrombotic events (32-34). Three forms of the SPS have been identified: Types I, II and III are defined by platelet hyperaggregability with both epinephrine and adenosine-diphosphate (ADP), type II with only epinephrine and type III with only ADP (13,31,35-39). The platelet abnormality appears to be congenital, based on familial occurrence, but the precise nature of the defect has not been defined. Treatment of SPS relies on diminishing the inherent platelet hyperaggregability by means of anti-platelet drugs; in most cases, aspirin appears adequate but there are situations in which other anti-platelet drugs must be employed (27,33,36,40-43) (see Table 1). Only one paper has described a prospective study of SPS treatment (40), and it proved that by using antiplatelet drugs, mainly aspirin, the platelet hyperreactivity of patients can be reverted and that this translates into a low re-thrombosis rate (36,40). Herein, we analyze the salient features of treatment of persons with SPS who have been identified in different parts of the world.
Table 1
| Author | Country | Year | Cases | Location of thrombosis | Treatment | Follow -up |
|---|---|---|---|---|---|---|
| Mammen |
USA | 1988 | Unknown | MI | Aspirin | Article not found |
| Berg-Dammer |
Germany | 1997 | 2 | Superior sagittal sinus/middle cerebral artery/left subclavian/left vertebral artery | Heparin/catheter/thrombolysis. Aspirin 100 mg/daily | Nineteen months after the failed attempt to treat the aneurysms, the patient had regained full working capability. At that time she was taking ASA (Aspirin) daily. A follow-up laboratory examination confirmed thrombocytosis as well as chronic intravasal activation of platelets, coagulation and fibrinolysis |
| Baker; Bick ( |
USA | 1999 | 153 | DVT/stroke/MI/retinal vein | Aspirin | – |
| Chaturvedi, Dzieczkowski ( |
USA | 1999 | 1 | Acute stroke | Heparin/Warfarin | – |
| Bick ( |
USA | 2000 | 21 | Recurrent miscarriage | Aspirin 81 mg/d | Immediately post-conception, fixed low dose subcutaneous heparin at 5,000 U (anti-Xa) every 12 hours was added to the daily ASA regimen 81 mg/d. The heparin used was Fuji porcine mucosal heparin (20,000 U/mL concentration). Two patients suffered loss on ASA plus heparin, and placental thrombi and infarcts were present; thus, there were two losses that clearly represented treatment failure |
| Weber |
Germany | 2002 | 34 | DVT/retinal vein thrombosis/portal vein thrombosis/pulmonary embolism | Heparin/Aspirin | – |
| Frenkel |
USA | 2003 | 200 | Acute stroke, DVT | Aspirin 81 mg/day | Treatment with low-dose aspirin reverses clinical symptoms and hyperaggregability in the laboratory |
| Lewerenz |
Germany | 2004 | 1 | Acute stroke/MI | Aspirin | – |
| Kahles |
Germany | 2006 | 1 | Acute myocardial infarction/pulmonary embolism | Abciximab/stent/antiplatelet therapy/t-PA/heparin | Despite intravenous full heparinization and platelet aggregation inhibition with acetylsalicylic acid 100 mg and ticlopidine 2×250 mg, the patient unexpectedly developed a cardiogenic shock after two days |
| Kubisz ( |
Slovakia | 2006 | 128 | Acute stroke/MI/DVT/recurrent miscarriage | – | – |
| Fodor |
Hungary | 2007 | 1 | Left temporal-superior branch retinal artery occlusion | Aspirin 300 mg/day | Four years after the event, her best-corrected visual acuity is stabilized at 20/20, without any further episodes of visual loss or any other neurological symptoms. The patient is under antiplatelet therapy (ASA: 100 mg/day) and undergoes imaging annually |
| Muhlfeld ( |
USA | 2007 | 3 | Renal allograft rejection/colonic microinfarctions/pulmonary embolism/DVT | Heparin/Aspirin 100 mg | In two cases, the patients and the affected family members were placed on low-dose acetylsalicylic acid therapy and platelet function tests normalized in successive testing. The other patient still developed vascular events while on therapy with acetylsalicylic acid |
| Randhawa |
New Zealand | 2007 | 1 | Ischemic optic neuropathy | Aspirin 81 mg/day | At 3-month follow up, his right optic disco edema had resolved |
| Ruiz-Argüelles |
Mexico | 2007 | 46 | Thrombosis at younger than 40/recurrent thrombosis/thrombosis in unusual sites | Aspirin | – |
| El-Amm |
USA | 2008 | 3 | Renal allograft rejection | Aspirin | – |
| Mears, Van Stavern ( |
USA | 2009 | 1 | Ischemic optic neuropathy | Aspirin 81 mg/day | – |
| Sand |
Germany | 2009 | 1 | Cutaneous microembolism on fingers | Heparin (does not mention the dose) | Despite heparin therapy |
| Bojalian |
USA | 2010 | 1 | Popliteal artery/renal and splenic infarction/left axillar artery/left subclavian artery/left internal jugular vein | Heparin/embolectomy/Aspirin | – |
| Loeffelbein |
Germany | 2010 | 1 | Venous and arterial flap thrombosis | Aspirin 81 mg/day | The treatment was well-tolerated, with no further thromboembolic events or problems |
| Alexandra |
USA | 2011 | 1 | Retinal vein | Aspirin (80–100 mg) | Given the possibility of recurrent thrombosis with oral anticoagulant therapy alone in patients with sticky platelet syndrome, she was concurrently maintained on low-dose aspirin therapy. On initial follow-up examination, the patient’s intraretinal hemorrhages remained stable, and there was no evidence of macular edema. She continues to deny any new visual symptoms or any decrease in visual acuity since that time. |
| Gehoff |
Germany | 2011 | 1 | Acute stroke, PFO | Aspirin (100 mg/day) | The analysis at 1 month demonstrated a therapeutic effect of the low-dose acetylsalicylic acid medication |
| Rac |
USA | 2011 | 1 | Recurrent miscarriage | Aspirin 325 mg/daily | She was subsequently started with ASA daily and has had no further clotting episodes. No treatment strategy, however, has been conclusively demonstrated to increase the chance of pregnancy success in patients with sticky platelet syndrome |
| Kotulicova |
Slovakia | 2012 | 77 | Pulmonary embolism/DVT/MI/Acute stroke | – | – |
| Kubisz |
Slovakia | 2012 | 9 | 2 DVT/4 arterial (acute stroke, MI, arterial thrombosis)/3 both | – | – |
| Sokol |
Slovakia | 2012 | 27 | Recurrent miscarriage | Aspirin | – |
| Darulova |
USA | 2013 | 1 | Pulmonary embolism | Alteplase/heparin was started with an intravenous bolus of alteplase 10 mg and then 40 mg intravenously during the first hour and 50 mg intravenously during the second hour. Intravenous anticoagulation with heparin was initiated after alteplase treatment to complete the treatment (heparin 10,000 U bolus and consequently 1,000 units/hour intravenously). This therapy was administrated with a positive effect and led to the stabilization of patient’s condition | This therapy was administrated with a positive effect and led to the stabilization of patient´s condition. After stabilization of patient´s condition, the cause of pulmonary embolism was investigated, but there was nothing in the history suggesting a cause |
| Ruiz-Argüelles |
Mexico | 2013 | 100 | Thrombosis at younger than 40/recurrent thrombosis/thrombosis in unusual sites | Aspirin | – |
| Simonova |
Slovakia | 2013 | 9 | Cerebral venous thrombosis/DVT/pulmonary embolism/acute stroke/MI | Heparin/Aspirin | – |
| Tekgunduz |
Turkey | 2013 | 6 | History of thrombosis | Aspirin 100 mg/day | – |
| Vasil’ev |
Russia | 2013 | 70 | Thrombosis | Heparin/Aspirin | Article not found |
| Castillo-Martinez |
Mexico | 2014 | 1 | Cutaneous limb veins | Aspirin 81 mg/day | She got a full recovery after four months |
| Hayes |
USA | 2014 | 64 | Acute stroke/DVT/MI | Aspirin | – |
| Kubisz ( |
Slovakia | 2014 | 71 | Acute stroke | – | – |
| Ruiz-Arguelles ( |
Mexico | 2014 | 95 | Thrombosis at younger than 40/recurrent thrombosis/thrombosis in unusual sites | Aspirin 81 mg/day | The platelet aggregation response to adenosine diphosphate and epinephrine significantly diminished after treatment and only two individuals developed another thrombosis, 52 and 129 months after starting therapy; interestingly, these two episodes were located in the retinal central artery and neither individual was identified to have any additional associated thrombophilic conditions |
| Alsheekh |
USA | 2015 | 1 | Carotid artery | Abciximab/thrombectomy (does not mention the dose) | A repeat duplex ultrasound was performed on postoperative day six and demonstrated a patent artery without a hemodynamically significant stenosis. At three year follow up the patient remained on dual antiplatelet therapy and without evidence of carotid occlusion. On follow-up at 7 years, patient remains well with no further neurologic events |
| Sokol |
Slovakia | 2015 | 23 | Recurrent miscarriage | Aspirin | – |
| Sokol |
Slovakia | 2015 | 27 | Recurrent miscarriage | Aspirin | – |
| Yagmur |
Germany | 2015 | 48 | TIA/DVT/pulmonary embolism/renal infarction | Heparin/Aspirin | – |
| Ruiz-Delgado |
Mexico | 2017 | 77 | Recurrent miscarriage | Aspirin | – |
| Skerenova |
Slovakia | 2018 | 37 | Recurrent miscarriage | Aspirin | – |
| Sokol |
Slovakia | 2018 | 64 | Recurrent miscarriage | Aspirin | – |
| Sokol |
Slovakia | 2018 | 84 | DVT | – | – |
| Solis-Jimenez |
Mexico | 2018 | 1 | Renal allograft rejection (renal infarction) | Nephrectomy/Aspirin | – |
MI, myocardial infarction; ASA, acetylsalicylic acid; DVT, deep vein thrombosis; TIA, transient ischemic attack; PFO, patent foramen oval.
Methods
We employed the PubMed database to search for all entries with the term “Sticky Platelet”, either in the title and/or the abstract. The relevant features of all publications were further analyzed, focusing in the treatment features and the re-thrombosis rate.
Results
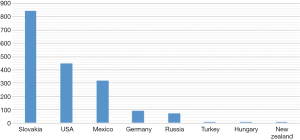
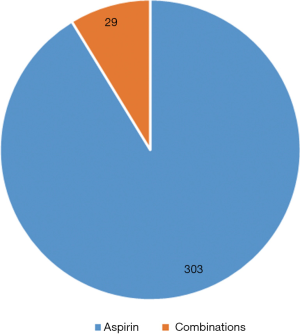
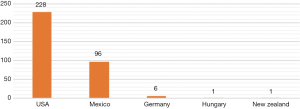
The initial search identified 108 papers in total. However, although 41 of these included the search terms, they were discarded as they did not actually describe SPS. Twenty-four papers comprised reviews on SPS and 43 papers described either cases or series of patients. These latter 43 papers (Table 1) were further assessed. The country with the greatest number of papers published on SPS was the United States (fourteen publications), followed by Slovakia (eleven publications), Germany (eight publications), and México (six publications), with Hungary, Turkey, Russia and New Zealand having only a single publication each (23,26,52,53) (see Figure 1). In these publications, a total of 1783 patients with SPS were identified over the past 30 years [1988–2019] (see Figure 2). The thromboses identified were both venous or arterial; in some patients, SPS was identified together with another thrombophilic condition, either acquired or inherited (10,25,39) (see Table 1). Three hundred thirty two patients were treated with antiplatelet drugs; 303 were given solely aspirin and 29 received combinations with aspirin (heparin or coumadin), whereas two persons did not receive aspirin (heparin + alteplase; abciximab) (see Figures 3 and 4).
The doses of aspirin employed ranged between 80 and 325 mg/day (see Table 1); information about the use of enteric-coated versus non-coated aspirin is unavailable. The re-thrombosis rate for patients given antiplatelet drugs was 5/325 (1.5%); two of these patients were given subsequently direct oral anticoagulants. In only two papers were platelet aggregometry studies repeated after the treatment, as a way to control the efficacy of the treatment (4,40).
Discussion
Over past years, we have been interested in analyzing the changes in the hemostatic system of Mexican Mestizos which can result in thrombophilia (40,42). In our studies, SPS was found to be the second most frequent thrombophilic condition identified in Mexican mestizos who expressed any clinical marker of thrombophilia (42), only exceeded by the MTHFR gene 677 C->T mutation. In México, we (11,19,24,42) and others (64) have found that approximately 50% of Mexican mestizo patients with a clinical maker of thrombophilia display the SPS phenotype. Most patients with SPS display other thrombosis-prone conditions, but there are also instances which SPS is identified as the single thrombophilia marker. Thus, SPS likely contributes to so-called “multifactorial thrombophilia” (19).
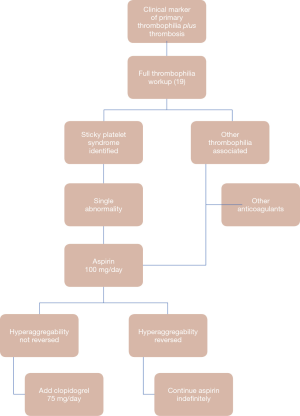
There are limited papers dealing with SPS treatment (Table 1); and most experiences stem from small series of patients or reviews (6,10,12,15,20,24,32,37,39,42,47-49,51,53,55,57-62,65-67) or case reports (4,8,17,21,23,25-30,34,44-46,50,52,54,56,63,68). Persons with the SPS phenotype but no history of thrombosis may not need treatment at all, but it is not irrational to prescribe them low doses of aspirin. For patients with history of thrombosis and the SPS phenotype, in a prospective study (40), we found that the platelet hyperaggregability can be reverted by means of aspirin in most cases (75%), whereas other/additional antiplatelet drugs were needed in the remaining 25% (with clopidogrel employed in our experience). Use of antiplatelet drugs enabled a low re-thrombosis rate at 129 months of 3.6%, thereby permitting freedom from re-thrombosis of 96.4% of the whole group of 55 patients at 129 months (40). The re-thrombosis rate that we found in our previous prospective study (3.6%), contrasts with that observed in the whole group of patients which we are presenting here (1.5%); this may stem from the fact that the data collection period in our group is substantially longer. In our prospective study (40), we analyzed the platelet hyperreactivity before and after the delivery of the antiplatelet drug and switched from aspirin to clopidogrel if the laboratory abnormally did not revert with aspirin (i.e., ‘aspirin resistance’ or ‘high on treatment aspirin activity’) (40). In another papers, we have suggested that pregnant women with the SPS phenotype should be given aspirin during all the pregnancy, mainly if they have experienced previous miscarriages (32,69,70). In the studies which we have now analyzed, only two (4,40) refer to repeating the platelet aggregation studies after starting antiplatelet drug therapy and then switching to another drug based on such testing; interestingly, despite the lack of any laboratory control of the treatment of persons with SPS, the re-thrombosis rate was very low (1.5%). This finding could militate against the recommendation of controlling the SPS treatment by means of platelet aggregometry studies but needs further investigation. There is no information available on the re-thrombosis rate in SPS patients not given antiplatelet drugs. Figure 5 refers to the algorithm that we suggest to treat patients with SPS, based on our experience and that stemming from the papers herein analyzed (19).
Conclusions
In summary, we have found that physicians worldwide are aware of the fact that the best treatment for persons with the SPS is the use of antiplatelet drugs. The rethrombosis rate is very low. Additional research on the SPS may be needed to better understand the pathophysiology of the condition; in the meanwhile, offering antiplatelet drugs to persons displaying the SPS phenotype seems adequate.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Emmanuel J. Favaloro) for the series “Anticoagulant and antithrombotic therapy: globally applied according to local geographical selection criteria” published in Annals of Blood. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aob.2019.06.05). The series “Anticoagulant and antithrombotic therapy: globally applied according to local geographical selection criteria” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Press M, Hartop PJ, Hawkey C. Proceedings: The correction of essential fatty acid deficiency and “sticky” platelets in man by the cutaneous administration of sunflower seed oil. Clin Sci Mol Med 1974;46:13P. [PubMed]
- Weston MJ, Langley PG, Williams R. Proceedings: Defective platelet function with deficiency of “sticky platelets” in fulminant hepatic failure. Gut 1975;16:405. [PubMed]
- Mammen EF, Barnhart MI, Selik NR, et al. “Sticky platelet syndrome”: a congenital platelet abnormality predisposing to thrombosis? Folia Haematol Int Mag Klin Morphol Blutforsch 1988;115:361-5. [PubMed]
- Berg-Dammer E, Henkes H, Trobisch H, et al. Sticky Platelet Syndrome: a Cause of Neurovascular Thrombosis and Thrombo-embolism. Interv Neuroradiol 1997;3:145-54. [Crossref] [PubMed]
- Chaturvedi S, Dzieczkowski J. Multiple hemostatic abnormalities in young adults with activated protein C resistance and cerebral ischemia. J Neurol Sci 1998;159:209-12. [Crossref] [PubMed]
- Baker WFJ, Bick RL. Treatment of hereditary and acquired thrombophilic disorders. Semin Thromb Hemost 1999;25:387-406. [Crossref] [PubMed]
- Mammen EF. Sticky platelet syndrome. Semin Thromb Hemost 1999;25:361-5. [Crossref] [PubMed]
- Chaturvedi S, Dzieczkowski JS. Protein S deficiency, activated protein C resistance and sticky platelet syndrome in a young woman with bilateral strokes. Cerebrovasc Dis 1999;9:127-30. [Crossref] [PubMed]
- Bick RL, Rice J. Long-term outpatient dalteparin (fragmin) therapy for arterial and venous thrombosis: efficacy and safety--a preliminary report. Clin Appl Thromb Hemost 1999;5:S67-71. [Crossref] [PubMed]
- Bick RL. Recurrent miscarriage syndrome due to blood coagulation protein/platelet defects: prevalence, treatment and outcome results. DRW Metroplex Recurrent Miscarriage Syndrome Cooperative Group. Clin Appl Thromb Hemost 2000;6:115-25. [Crossref] [PubMed]
- Ruiz-Argüelles GJ, Lopez-Martinez B, Cruz-Cruz D, et al. Primary thrombophilia in Mexico III: A prospective study of the sticky platelet syndrome. Clin Appl Thromb Hemost 2002;8:273-7. [Crossref] [PubMed]
- Weber M, Gerdsen F, Gutensohn K, et al. Enhanced platelet aggregation with TRAP-6 and collagen in platelet aggregometry in patients with venous thromboembolism. Thromb Res 2002;107:325-8. [Crossref] [PubMed]
- Ruiz-Argüelles GJ, Ruiz-Delgado GJ, López-Martínez B. The sticky platelet syndrome: a frequent but unrecognized cause of thrombophilia. Rev Invest Clin 2002;54:394-6. [PubMed]
- Bick RL. Prothrombin G20210A mutation, antithrombin, heparin cofactor II, protein C, and protein S defects. Hematol Oncol Clin North Am 2003;17:9-36. [Crossref] [PubMed]
- Frenkel EP, Mammen EF. Sticky platelet syndrome and thrombocythemia. Hematol Oncol Clin North Am 2003;17:63-83. [Crossref] [PubMed]
- Lazo-Langner A. Sticky platelet syndrome. Rev Invest Clin 2004;56:103-4. [PubMed]
- Lewerenz V, Burchardt T, Buchau A, et al. Livedoid vasculopathy with heterozygous factor V Leiden mutation and sticky platelet syndrome. Hautarzt 2004;55:379-81. [Crossref] [PubMed]
- Bick RL, Hoppensteadt D. Recurrent miscarriage syndrome and infertility due to blood coagulation protein/platelet defects: a review and update. Clin Appl Thromb Hemost 2005;11:1-13. [Crossref] [PubMed]
- Ruiz-Argüelles GJ, Lopez-Martinez B, Valdes-Tapia P, et al. Primary thrombophilia in Mexico. V. A comprehensive prospective study indicates that most cases are multifactorial. Am J Hematol 2005;78:21-6. [Crossref] [PubMed]
- Kubisz P, Ivankov J, Holly P, et al. The glycoprotein IIIa PL(A1/A2) polymorphism--a defect responsible for the sticky platelet syndrome? Clin Appl Thromb Hemost 2006;12:117-9. [Crossref] [PubMed]
- Kahles H, Trobisch H, Kehren H. Disseminated coronary occlusions and massive pulmonary embolism in a 40-year-old woman. Dtsch Med Wochenschr 2006;131:672-5. [Crossref] [PubMed]
- Andersen J. Sticky platelet syndrome. Clin Adv Hematol Oncol 2006;4:432-4. [PubMed]
- Fodor M, Facsko A, Berenyi E, et al. Transient visual loss triggered by scuba diving in a patient with a petrous epidermoid and combined thrombotic risk factors. Pathophysiol Haemost Thromb 2007;36:311-4. [Crossref] [PubMed]
- Ruiz-Argüelles GJ, Gonzalez-Carrillo ML, Estrada-Gomez R, et al. Primary thrombophilia in Mexico. VI: lack of statistical association among the inherited thrombophilic conditions. Gac Med Mex 2007;143:317-22. [PubMed]
- Mühlfeld AS, Ketteler M, Schwamborn K, et al. Sticky platelet syndrome: an underrecognized cause of graft dysfunction and thromboembolic complications in renal transplant recipients. Am J Transplant 2007;7:1865-8. [Crossref] [PubMed]
- Randhawa S, Van Stavern GP. Sticky platelet syndrome and anterior ischaemic optic neuropathy. Clin Exp Ophthalmol 2007;35:779-81. [Crossref] [PubMed]
- El-Amm JM, Andersen J, Gruber SA. Sticky platelet syndrome: a manageable risk factor for posttransplant thromboembolic events. Am J Transplant 2008;8:465. [Crossref] [PubMed]
- Sand M, Mann B, Bechara FG, et al. Sticky platelet syndrome type II presenting with arterial microemboli in the fingers. Thromb Res 2009;124:244. [Crossref] [PubMed]
- Mears KA, Van Stavern GP. Bilateral simultaneous anterior ischaemic optic neuropathy associated with Sticky Platelet Syndrome. Br J Ophthalmol 2009;93:885-886,913. [Crossref] [PubMed]
- Loeffelbein DJ, Baumann CM, Mucke T, et al. Sticky platelet syndrome as a possible cause for free flap failure--a case report. Microsurgery 2010;30:466-8. [Crossref] [PubMed]
- Vallejo-Villalobos MF, Gómez-Cruz GB, Cantero-Fortiz Y, et al. Primary thrombophilia XIV. Worldwide identification of the Sticky Platelet Syndrome. Semin Thromb Hemost 2019;45:423-8. [Crossref] [PubMed]
- Ruiz-Delgado GJ, Cantero-Fortiz Y, Mendez-Huerta MA, et al. Primary Thrombophilia in Mexico XII: Miscarriages Are More Frequent in People with Sticky Platelet Syndrome. Turk J Haematol 2017;34:239-43. [PubMed]
- Ruíz-Argüelles GJ, Alarcón-Urdaneta C, Calderón-García J, et al. Primary thrombophilia in México VIII: Description of five kindreds of familial sticky platelet syndrome phenotype. Rev Hematol Mex 2011;12:73-8.
- Rac MWF, Minns Crawford N, Worley KC. Extensive Thrombosis and First-Trimester Pregnancy Loss Caused by Sticky Platelet Syndrome. Obstet & Gynecol 2011;117:501-3. [Crossref] [PubMed]
- Kubisz P, Stasko J, Holly P. Sticky platelet syndrome. Semin Thromb Hemost 2013;39:674-83. [Crossref] [PubMed]
- Moncada B, Ruíz-Arguelles GJ, Castillo-Martinez C. The sticky platelet syndrome. Hematology 2013;18:230-2. [Crossref] [PubMed]
- Kubisz P. Response to “Comment on Sticky platelet syndrome”. Seminars in thrombosis and hemostasis 2014;40:274. [Crossref] [PubMed]
- Kubisz P, Ruiz-Arguelles GJ, Stasko J, et al. Sticky platelet syndrome: history and future perspectives. Semin Thromb Hemost 2014;40:526-34. [Crossref] [PubMed]
- Ruiz-Arguelles GJ. Comment on Sticky platelet syndrome. Semin Thromb Hemost 2014;40:273. [Crossref] [PubMed]
- Velázquez-Sánchez-de-Cima S, Zamora-Ortiz G, Hernandez-Reyes J, et al. Primary thrombophilia in Mexico X: a prospective study of the treatment of the sticky platelet syndrome. Clin Appl Thromb Hemost 2015;21:91-5. [Crossref] [PubMed]
- Kubisz P, Holly P, Stasko J. Sticky Platelet Syndrome: 35 Years of Growing Evidence. Semin Thromb Hemost 2019;45:61-8. [Crossref] [PubMed]
- Ruiz-Argüelles GJ, Garces-Eisele J, Camacho-Alarcon C, et al. Primary thrombophilia in Mexico IX: the glycoprotein IIIa PLA1/A2 polymorphism is not associated with the sticky platelet syndrome phenotype. Clin Appl Thromb Hemost 2013;19:689-92. [Crossref] [PubMed]
- Calderón-Cruz B, Pérez-González A, Peña-Duque MA, et al. Prasugrel resistance may be linked to the sticky platelet syndrome report of one case. Rev Hematol Mex 2011;12:105-9.
- Bojalian MO, Akingba AG, Andersen JC, et al. Sticky platelet syndrome: an unusual presentation of arterial ischemia. Ann Vasc Surg 2010;24:691.e1 [Crossref] [PubMed]
- Alexandra AO, Drenser KA. Hypercoagulable state in a patient with a retinal vein occlusion. Retin Cases Brief Rep 2011;5:76-8. [Crossref] [PubMed]
- Gehoff A, Kluge JG, Gehoff P, et al. Recurrent strokes under anticoagulation therapy: Sticky platelet syndrome combined with a patent foramen ovale. J Cardiovasc Dis Res 2011;2:68-70. [Crossref] [PubMed]
- Kotuličová D, Chudy P, Skerenova M, et al. Variability of GP6 gene in patients with sticky platelet syndrome and deep venous thrombosis and/or pulmonary embolism. Blood Coagul Fibrinolysis 2012;23:543-7. [Crossref] [PubMed]
- Kubisz P, Ivankova J, Skerenova M, et al. The prevalence of the platelet glycoprotein VI polymorphisms in patients with sticky platelet syndrome and ischemic stroke. Hematology 2012;17:355-62. [Crossref] [PubMed]
- Sokol J, Biringer K, Skerenova M, et al. Platelet aggregation abnormalities in patients with fetal losses: the GP6 gene polymorphism. Fertil Steril 2012;98:1170-4. [Crossref] [PubMed]
- Darulová S, Samos M, Sokol J, et al. Sticky platelets syndrome in a young patient with massive pulmonary embolism. Am J Case Rep 2013;14:169-72. [Crossref] [PubMed]
- Šimonová R, Bartosova L, Chudy P, et al. Nine kindreds of familial sticky platelet syndrome phenotype. Clin Appl Thromb Hemost 2013;19:395-401. [Crossref] [PubMed]
- Tekgündüz E, Demir M, Akyol Erikci A, et al. Sticky platelet syndrome in patients with uninduced venous thrombosis. Turk J Haematol 2013;30:48-52. [PubMed]
- Vasil’ev SA, Vinogradov VL, Gemdzhian EG, et al. Experience with outpatient treatment for thromboses and thrombophilias. Ter Arkh 2013;85:47-50. [PubMed]
- Castillo-Martínez C, Moncada B, Valdes-Rodriguez R, et al. Livedoid vasculopathy (LV) associated with sticky platelets syndrome type 3 (SPS type 3) and enhanced activity of plasminogen activator inhibitor (PAI-1) anomalies. Int J Dermatol 2014;53:1495-7. [Crossref] [PubMed]
- Hayes C, Kitahara S, Tcherniantchouk O. Decreased Threshold of Aggregation to Low-Dose Epinephrine is Evidence of Platelet Hyperaggregability in Patients with Thrombosis. Hematol Rep 2014;6:5326. [Crossref] [PubMed]
- Alsheekh AA, Puggioni A, Hingorani AP, et al. The sticky platelet syndrome during carotid endarterectomy. Ann Vasc Surg 2015;29:1317.e9-1317.e11. [Crossref] [PubMed]
- Sokol J, Biringer K, Skerenova M, et al. Different models of inheritance in selected genes in patients with sticky platelet syndrome and fetal loss. Semin Thromb Hemost 2015;41:330-5. [Crossref] [PubMed]
- Sokol J, Skerenova M, Biringer K, et al. Genetic variations of the GP6 regulatory region in patients with sticky platelet syndrome and miscarriage. Expert Rev Hematol 2015;8:863-8. [Crossref] [PubMed]
- Yagmur E, Frank RD, Neulen J, et al. Platelet Hyperaggregability is Highly Prevalent in Patients With Chronic Kidney Disease: An Underestimated Risk Indicator of Thromboembolic Events. Clin Appl Thromb Hemost 2015;21:132-8. [Crossref] [PubMed]
- Škereňová M, Sokol J, Biringer K, et al. GP6 Haplotype of Missense Variants is Associated with Sticky Platelet Syndrome Manifested by Fetal Loss. Clin Appl Thromb Hemost 2018;24:63-9. [Crossref] [PubMed]
- Sokol J, Skerenova M, Biringer K, et al. Glycoprotein VI Gene Variants Affect Pregnancy Loss in Patients With Platelet Hyperaggregability. Clin Appl Thromb Hemost 2018;2018:1076029618802358 [PubMed]
- Sokol J, Skerenova M, Ivankova J, et al. Association of Genetic Variability in Selected Genes in Patients With Deep Vein Thrombosis and Platelet Hyperaggregability. Clin Appl Thromb Hemost 2018;24:1027-32. [Crossref] [PubMed]
- Solis-Jimenez F, Hinojosa-Heredia H, Garcia-Covarrubias L, et al. Sticky Platelet Syndrome: An Unrecognized Cause of Acute Thrombosis and Graft Loss. Case Rep Nephrol 2018;2018:3174897 [Crossref] [PubMed]
- Hernández-Hernández D, Villa R, Murillo-Bonilla LM, et al. Hiperagregabilidad plaquetaria y síndrome de plaquetas pegajosas (SPP) en eventos vasculares cerebrales en jóvenes. Rev Hematol Mex 2002;3:19.
- Salvagno GL, Pavan C, Lippi G. Rare thrombophilic conditions. Ann Transl Med 2018;6:342. [Crossref] [PubMed]
- Favaloro EJ, Lippi G. Commentary: Controversies in Thrombosis and Hemostasis Part 2-Does Sticky Platelet Syndrome Exist? Semin Thromb Hemost 2019;45:69-72. [Crossref] [PubMed]
- Azamar-Solis B, Cantero-Fortiz Y, Olivares-Gazca JC, et al. Primary Thrombophilia in Mexico XIII: Localization of the Thrombotic Events in Mexican Mestizos With the Sticky Platelet Syndrome. Clin Appl Thromb Hemost 2019;25:1076029619841700 [Crossref] [PubMed]
- Kubisz P, Kotulicova D, Chudy P, et al. Sticky platelet syndrome in a patient with transitory ischemic attack and the family. A case report. Rev Hematol Mex 2011;12:99-104.
- Kubisz P, Stanciakova L, Stasko J, et al. Sticky platelet syndrome: an important cause of life-threatening thrombotic complications. Expert Rev Hematol 2016;9:21-35. [Crossref] [PubMed]
- Sokol J, Skerenova M, Jedinakova Z, et al. Progress in the Understanding of Sticky Platelet Syndrome. Semin Thromb Hemost 2017;43:8-13. [PubMed]
Cite this article as: García-Navarrete YI, Vallejo-Villalobos MF, Olivares-Gazca JM, Cantero-Fortiz Y, León-Peña AA, Olivares-Gazca JC, Murrieta-Álvarez I, Ruiz-Delgado GJ, Ruiz-Argüelles GJ. Primary thrombophilia XV: antithrombotic treatment of sticky platelet syndrome worldwide. Ann Blood 2019;4:15.



