
Large number of blood donors have hypertension based on the updated 2017 hypertension guidelines
Introduction
Blood donors are considered to be a healthy population or healthier group of people. As part of donor screening, blood pressures are measured in potential donors before each donation.
In 2017 the American College of Cardiology (ACC) and American Heart Association (AHA) published updated hypertension guidelines with new criteria for the definition of hypertension (1). Normal blood pressure is defined as below 120/80 mmHg. Systolic blood pressure (SBP) above 130 mmHg or diastolic blood pressure (DBP) above 80 mmHg are now diagnosed as hypertension in contrast to the 140/90 mmHg criteria, as established in the Seventh Report guidelines by the Joint National Committee (JNC7) (2).
In this study, we determined the prevalence of hypertension among blood donors at a large regional blood donation center, Bloodworks Northwest (NW) in the Pacific Northwest, using the updated 2017 ACC/AHA guidelines. We then examined the proportion of hypertension in different subsets of donors, further categorized by gender, age and ethnicity. These donor subgroups were subsequently compared with their national counterparts. We present the following article in accordance with the MDAR checklist (available at http://dx.doi.org/10.21037/aob-20-12).
Methods
Donation records (de-identified) from January 1, 2017 to December 31, 2017 were retrieved from the centralized database at Bloodworks NW. Directed, autologous, and therapeutic donations were excluded. Only donors who made voluntary donations of whole blood or apheresis donations of red cells, platelets or plasma were included. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Western Institutional Review Board (WIRB) review board (No. IRB00000533) and informed consent was waived because of minimal risk. Before blood pressure readings were taken, potential blood donors would first register for blood donation and then sit down to fill out a questionnaire followed by a sit-down interview for confirmation of donor information and answers to blood donation survey. Blood pressures were measured using validated and calibrated sphygmomanometers by trained phlebotomists, following the blood donation center’s standard operating procedure for pre-donation blood pressure measurements.
Donor’s age, sex, ethnicity, and measured blood pressure (SBP and DBP) from the first donation of the year were collected. A single blood pressure measurement was captured for each donation. Blood pressures of donors were characterized into 4 groups (normal blood pressure, elevated blood pressure, stage 1 hypertension or stage 2 hypertension) according to the 2017 ACC/AHA hypertension guidelines (1).
Donors were then divided into different subsets in the same manner as the published analysis of National Health and Nutrition Examination Survey by Muntner et al. (3). Five different age groups were created: 20–44 years of age, 45–54 years, 55–64 years, 65–74 years or >75 years. Ethnicity was classified as non-Hispanic whites, non-Hispanic blacks, non-Hispanic Asians, or Hispanic. Hypertension percentages of the various subgroups of blood donors at Bloodworks NW were then compared to the US population estimates as determined by Muntner et al. (3).
Statistical analysis
Data extraction was performed by Tableau Desktop (Seattle, WA), Microsoft Access (Redmond, WA), and Microsoft Excel (Redmond, WA). Analysis was performed using statistical software, RStudio v1.0.136 with R version 3.4.3 (Boston, MA). We utilized bootstrapping to better understand the accuracy of our sampling estimates. Bootstrapping falls under the broader category of resampling methods. In this study, we generated 95% confidence intervals by resampling our dataset 1,000 times, computing the percentage of those with hypertension, and then calculating the normal statistics of the resulting distribution.
Results
For one year from January 1, 2017 to December 31, 2017, 116,270 potential donors presented at Bloodworks NW in the Pacific Northwest. Blood pressures were measured and recorded before each attempted blood donation. Forty-four percent of the donors donated 2 or more times during that year, and for those donors, only the blood pressure from the first donation of the year was used for the study.
Tables 1 and 2 summarize the SBP and DBP readings of all blood donors at Bloodworks NW in 2017. The mean and median SBP was at or above 120 mmHg except for the female donors. The mean and median DBP was under 80 mmHg except for the median DBP (80 mmHg) in male donors. However, a high percentage of donors (57.4% and 44.9%, respectively) did not have normal SBP (<120 mmHg) nor normal DBP (<80 mmHg).
Table 1
| Systolic blood pressure | Number of donors | Average SBP (mmHg) | Median SBP (mmHg) | 2.5th to 97.5th percentile (mmHg) | % of donors with SBP ≥120 |
|---|---|---|---|---|---|
| All donors | 116,270 | 122 | 120 | 98–158 | 57.4 |
| Female donors | 63,722 | 119 | 118 | 94–152 | 47.3 |
| Male donors | 52,548 | 126 | 124 | 100–160 | 69.7 |
Table 2
| Diastolic blood pressure | Number of donors | Average DBP (mmHg) | Median DBP (mmHg) | 2.5th to 97.5th percentile (mmHg) | % of donors with DBP ≥80 |
|---|---|---|---|---|---|
| All donors | 116,270 | 77 | 78 | 59–100 | 44.9 |
| Female donors | 63,722 | 75 | 76 | 58–97 | 37.3 |
| Male donors | 52,548 | 79 | 80 | 60–100 | 54.1 |
Table 3 lists the percentage of donors in each of the subgroups that met the criteria for normal blood pressure (SBP <120 mmHg and DBP <80 mmHg), elevated blood pressure (SBP 120–129 mmHg and DBP <80 mmHg), stage I hypertension (SBP 130–139 mmHg or DBP 80–89 mmHg) and stage 2 hypertension (SBP ≥140 mmHg or DBP ≥90 mmHg) (1). Total hypertension represents the combination of the stage 1 and stage 2 hypertension groups.
Table 3
| Variable | Total number of donors | Blood pressure | Stage | ||||
|---|---|---|---|---|---|---|---|
| Normal blood pressure | Elevated blood pressure | Stage I hypertension | Stage II hypertension | Total hypertension (stage 1 + stage2)/95% confidence interval | |||
| All donors | 116,270 | 35.1% | 13.2% | 31.9% | 19.8% | 51.7%/51.5–52.0% | |
| Gender | |||||||
| Male | 52,548 | 23.4% | 13.8% | 35.9% | 27.0% | 62.9%/62.5–63.3% | |
| Female | 63,722 | 44.8% | 12.6% | 28.6% | 14% | 42.6%/42.2–43.0% | |
| Age | |||||||
| 20–44 | 44,662 | 40.7% | 12.2% | 31.6% | 15.6% | 47.2%/46.7–47.6% | |
| 45–54 | 17,661 | 30.6% | 10.2% | 35.3% | 23.9% | 59.2%/58.5–59.9% | |
| 55–64 | 19,884 | 25.5% | 12.6% | 34.5% | 27.4% | 61.8%/61.2–62.5% | |
| 65–74 | 11,657 | 21.5% | 15.3% | 32.7% | 30.5% | 63.2%/62.3–64.0% | |
| ≥75 | 2,935 | 17.4% | 17.4% | 31.4% | 33.7% | 65.1%/63.4–66.8% | |
| Race/ethnicity | |||||||
| Caucasian | 88,196 | 34.1% | 13.3% | 32.3% | 20.3% | 52.7%/52.3–53.0% | |
| Black | 1,826 | 34.7% | 12.0% | 32.4% | 20.9% | 53.3%/50.9–55.6% | |
| Asian | 7,692 | 42.7% | 10.8% | 30.0% | 16.6% | 46.6%/45.4–47.7% | |
| Hispanic | 4,868 | 42.4% | 12.5% | 31.1% | 14.0% | 45.0%/43.7–46.4% | |
The percentage of hypertensive male donors was 62.9% versus 42.6% of female donors. Not surprisingly, the percentage of total hypertension grew with increasing age, but it was alarming to find 47.2% hypertension in the youngest age group analyzed (20–44 years of age). The overwhelming majority of our donors were non-Hispanic whites, constituting 76% of all our donors. The total percentage of hypertension ranged from 45.0% in Hispanic group to 53.3% in the non-Hispanic black group. The non-Hispanic white and Asian donor groups showed 52.7% and 46.6% hypertension, respectively.
Comparison to US population at large
Muntner et al. analyzed blood pressure data from the 2011 to 2014 National Health and Nutrition Examination Survey and weighted the results to generate US population estimates (3). We compared the blood pressure data of the blood donors to the US population at large (Table 4). Figure 1A,B,C compare the percentages of hypertension between the various subgroups of blood donors and their population counterparts.
Table 4
| Variable | Blood donors at Bloodworks Northwest (95% confidence interval) | US population at large (95% confidence interval) |
|---|---|---|
| Overall | 51.7% (51.5–52.0%) | 45.6% (43.6–47.6%) |
| Gender | ||
| Male | 62.9% (62.5–63.3%) | 48.6% (45.9–51.3%) |
| Female | 42.6% (42.2–43.0%) | 42.9% (40.7–45.1%) |
| Age group | ||
| 20–44 | 47.2% (46.7–47.6%) | 24.0% (21.8–26.2%) |
| 45–54 | 59.2% (58.5–59.9%) | 47.1% (44.4–49.8%) |
| 55–64 | 61.8% (61.2–62.5%) | 66.6% (63.6–69.5%) |
| 65–74 | 63.2% (62.3–64.0%) | 75.6% (73.4–77.6%) |
| ≥75 | 65.1% (63.4–66.8%) | 82.3% (79.2–85.0%) |
| Race/ethnicity | ||
| Non-Hispanic whites | 52.7% (52.3–53.0%) | 47.3% (44.5–50.0%) |
| Non-Hispanic blacks | 53.3% (50.9–55.6%) | 54.9% (52.5–57.3%) |
| Non-Hispanic Asians | 46.6% (45.4–47.7%) | 36.7% (32.6–40.9%) |
| Hispanic | 45.0% (43.7–46.4%) | 34.4% (31.8–37.1%) |
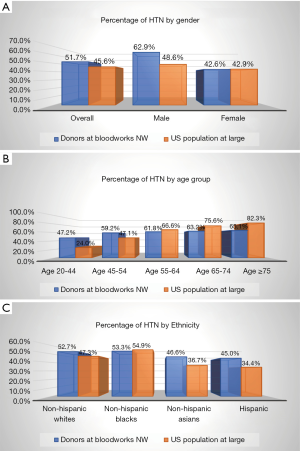
The biggest difference was in the 20–44 age group where 47.2% of blood donors were hypertensive compared to 24.0% of the same age group in the population at large (Figure 1B). In contrast, the older blood donors fared better than their population counterparts in terms of blood pressure; for 65–74 and over 75 age groups, 63.2% and 65.1% of blood donors were hypertensive versus 75.6% and 82.3% of the general population, respectively.
Of male blood donors, 62.9% were deemed hypertensive in contrast to 48.6% in the general population (Figure 1A). Female donors fared better with hypertension in 42.6%, which was very comparable to the general female population of 42.9%.
Except for the non-Hispanic black donor subgroup, the other three ethnic groups of blood donors showed higher percentages of hypertension than their population counterparts, higher by about 5–10% (Figure 1C). A slightly lower percentage of the non-Hispanic black donors at Bloodworks NW had hypertension in comparison to their population counterparts (53.3% versus 54.9%, respectfully). We were not able to assess the statistical significance of this difference.
Blood donors in this study comprised a cosmopolitan, ethnically diverse population in the Pacific Northwest region of the United States. A significant number of blood donors had elevated blood pressures based on the updated hypertension guidelines of 2017. Overall, 51.7% of all blood donors at Bloodworks NW who presented for blood donation in 2017 were deemed hypertensive, and 35.1% had normal blood pressure. When we compared blood donor subgroups with that of the national population, the percentage of hypertension among donors at Bloodworks NW was generally higher than their national counterparts except for the female donors that showed a comparable percentage of hypertension with women in the general population. The percentage of hypertension in male donors of 62.9% was higher than the 48.6% in their national counterpart. The percentage of hypertension of 47.2% of our younger donors in 20–44-year-old group was substantially higher than the hypertension percentage of 24.0% in the same age group in the general population. Interestingly, the non-Hispanic black blood donors had a slightly lower hypertension percentage of 53.3% compared to 54.9% of their national counterparts. African American donors constituted only 1.6% of all blood donors, and 73% of them were under 45 years of age.
Blood pressure in the pre-donation step is generally measured once per standard operating procedures, and lack of two measurements on separate days may be considered a limitation to this study. In addition, the statistical significance of the differences noted in the percentage of hypertension between the blood donor subgroups and their national counterparts cannot be assessed because the US population estimates were determined by calculations using sampling weights.
Although blood donors are generally considered “healthy,” more than 50% of blood donors at Bloodworks NW may be considered hypertensive according to the updated 2017 ACC/AHA guidelines. This unexpected high prevalence indicates the need for more studies on a national and international level to confirm the findings in this study and to assess the need for further action to promote donor health. In addition, depending on the region, up to 10% of population comprised of different ethnic groups are blood donors (4), therefore health promotion in blood donors can be an effective means in preventive care.
Although blood pressure is only one of multiple parameters of cardiovascular health, hypertension is a modifiable risk factor that can generate large gains in overall health when blood pressure is controlled. Blood pressure screening is one of the required measurements before blood donation can occur. Therefore, blood donation centers can serve as a hypertension screening vehicle for donors. They can help educate donors about hypertension and encourage them to modify life styles or seek medical treatment for hypertension. Blood donors in one study found that distribution of an informational sheet on hypertension was valuable (5). In addition to screening donors and improving education, donors can be encouraged to reach out to friends, family, and coworkers about hypertension. In so doing, donors can become advocates for hypertension awareness and be a vehicle for hypertension prevention within the greater community.
Conclusions
Significant percentage of hypertension among blood donors indicates a need and an opportunity for blood donation centers to improve donor health through blood pressure screening and education on hypertension.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MDAR checklist. Available at http://dx.doi.org/10.21037/aob-20-12
Data Sharing Statement: http://dx.doi.org/10.21037/aob-20-12
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aob-20-12). Dr. YW serves as an unpaid editorial board member of Annals of Blood. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Western Institutional Review Board (WIRB) review board (No. IRB00000533) and informed consent was waived because of minimal risk.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:1269-324. [Crossref] [PubMed]
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206-52. [Crossref] [PubMed]
- Muntner P, Carey RM, Gidding S, et al. Potential US Population Impact of the 2017 ACC/AHA High Blood Pressure Guideline. Circulation 2018;137:109-18. [Crossref] [PubMed]
- Yazer MH, Delaney M, Germain M, et al. Trends in US minority red blood cell unit donations. Transfusion 2017;57:1226-34. [Crossref] [PubMed]
- Hao J, McAvoy J, Wickberg L, et al. Is blood donation an opportunity for hypertension awareness?. Transfus Med 2016;26:89-98. [Crossref] [PubMed]
Cite this article as: Housekeeper J, Huang J, Chen E, Li L, Wu Y. Large number of blood donors have hypertension based on the updated 2017 hypertension guidelines. Ann Blood 2020;5:24.


