Management of immune thrombocytopenia in pregnancy
Introduction
Immune thrombocytopenia (ITP) occurs in 0.83 of 10,000 pregnancies (1) and presents unique challenges in the peripartum setting. ITP can develop at any time point during pregnancy and can be difficult to distinguish from other causes of thrombocytopenia in pregnancy such as gestational thrombocytopenia (GT), acute fatty liver of pregnancy and the hypertensive emergencies (preeclampsia and HELLP; hemolysis, elevated liver enzymes, low platelet count) (1,2). Women with pre-existing ITP may have worsening disease during pregnancy, nearly half requiring treatment (2). Treatment of peripartum ITP is indicated depending on signs of bleeding, the degree of thrombocytopenia and clinical course of the pregnancy; higher platelet count treatment thresholds are required as the mother approaches delivery and is at higher risk for bleeding (3). Careful monitoring of the mother throughout pregnancy is critical to avoid risk to both the mother and neonate. In this review, diagnosis and care of women with peripartum ITP will be discussed.
Diagnosis
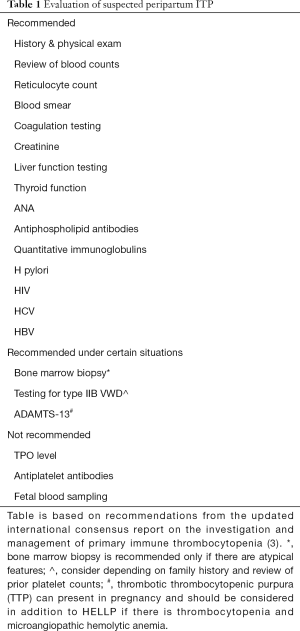
Similar to the non-pregnant patient, peripartum ITP is a diagnosis of exclusion; there is no definitive diagnostic test for ITP and presentations can be similar to other causes of thrombocytopenia. Thrombocytopenia should first be confirmed by reviewing the peripheral smear to exclude pseudothrombocytopenia or platelet clumping (Table 1). ITP is diagnosed after other causes of acquired thrombocytopenia are excluded such as drug induced thrombocytopenia, cirrhosis and splenic sequestration. Inherited thrombocytopenia should be considered in patients with longstanding thrombocytopenia and inadequate platelet count responses to glucocorticoids and/or intravenous immunoglobulin (IVIG). An absence of a family history of thrombocytopenia does not definitely rule inherited thrombocytopenia as some are autosomal recessive and de novo mutations can occur.
Causes of thrombocytopenia unique to pregnancy must also be considered when diagnosing ITP in the peripartum setting (3). Over the course of normal pregnancy, platelet counts decline due to increased blood volume and cell turn over (4,5). In 5–10% of healthy pregnancies, women develop thrombocytopenia beyond the normal decline in pregnancy due to GT (4,5). GT is the most common cause of thrombocytopenia in pregnancy and most cases are benign with counts generally above 100×109/L (5). GT often develops in later pregnancy, most frequently immediately prior to delivery (5). It can be difficult to distinguish GT from mild ITP, particularly if thrombocytopenia occurs in the first trimester when ITP is the most common cause of thrombocytopenia in pregnancy (5,6). Unlike ITP, thrombocytopenia of GT will not respond to IVIG or glucocorticoids (7). If the mother does not require treatment, postpartum monitoring may help differentiate as GT will resolve after delivery (8). Although there are rare reports of GT associated with neonatal thrombocytopenia (8), other causes of neonatal thrombocytopenia must be excluded, including neonatal alloimmune thrombocytopenia (NAITP) (9). Mild forms of inherited thrombocytopenia and type IIB von Willebrand disease can present in the mother during pregnancy and then be associated with neonatal thrombocytopenia. Obtaining pre-pregnancy platelet counts and an extensive family and bleeding history is critical for diagnosis.
Additional causes of thrombocytopenia unique to pregnancy include preeclampsia, HELLP syndrome (hemolysis, elevated liver enzymes, low platelet count), and acute fatty liver of pregnancy. Signs and symptoms of preeclampsia should be evaluated particularly if the patient develops thrombocytopenia late in pregnancy. Presence of preeclampsia does not exclude a concurrent diagnosis of ITP depending on the patient’s history. Furthermore, women with pre-existing ITP can develop pregnancy complications such as preeclampsia or HELLP syndrome.
Although common in pregnancy, anemia should be evaluated beyond iron studies in women with concurrent thrombocytopenia. Testing should include a blood smear and laboratory testing to rule out hemolysis. Concurrent immune mediated hemolysis suggests Evans syndrome. Thrombotic microangiopathies (TMA) should be considered if there is microangiopathic hemolytic anemia and thrombocytopenia. While HELLP is a pregnancy related TMA, both hemolytic uremic syndrome and thrombotic thrombocytopenic purpura can present in pregnancy. Abnormalities of other cell lines or organ dysfunction may suggest a bone marrow failure syndrome.
Distinguishing ITP from other causes of thrombocytopenia can be diagnostically challenging. Increased platelet counts with glucocorticoids and/or IVIG suggests ITP, but cannot distinguish between primary and secondary ITP. Primary or idiopathic ITP has no known associated disorder. Secondary ITP is ITP associated with an underlying disorder such as a hepatitis C, HIV, rheumalogic disorders (e.g., systemic lupus erythematous), or a lymphoproliferative disorder. Treating the underlying disorder may resolve thrombocytopenia in secondary ITP.
Diagnostic testing in ITP
Bone marrow biopsy is not required for diagnosis of ITP including in the peripartum setting (3), however, it may be required if there is concern for marrow failure or hematologic malignancy, or if the patient does not have an appropriate response to ITP directed therapies (Table 1).
Currently available tests for antiplatelet antibodies have poor sensitivity and specificity and testing is recommended only in the research setting (3). The presence of anti-platelet antibodies does not alter management, nor prognosticate the course of the mother or neonate. While ITP is thought to be primarily an autoantibody driven disease, direct T cell cytotoxicity likely contributes and is not captured with antibody testing (10).
Thrombopoietin (TPO) levels appear to be elevated in patients with ITP during pregnancy (11), however TPO testing is currently not routinely available and not recommended (3) (Table 1). In the non-pregnant population, higher TPO levels correlate with non-response to TPO receptor agonists (TPORAs) (12). In the pregnancy setting, TPO levels have not been shown to predict the severity of ITP and it is unknown if TPO levels predict response to recombinant TPO or TPORAs.
Immune changes in pregnancy
Pregnancy induced immunomodulation undoubtedly impacts ITP and new onset ITP during pregnancy likely represents a form of secondary ITP. Complex immune changes occur both systemically and at the maternal fetal interface at the placenta, allowing the maternal immune system to tolerate paternal alloantigens. Reduced exposure to paternal human leukocyte antigens (HLA) may be critical for tolerance; fetal extravillous trophoblasts that migrate into the decidual lack expression of classical HLA class Ia and class II molecules and instead have non classical HLA class Ib molecules (13,14). Maternal tolerance is also regulated by hormones such as increased progesterone and beta HCG, which promote maternal immune cells to shift from an inflammatory (Th1) to regulatory (Th2) cytokine profile (15). While immunomodulation of pregnancy promotes tolerance of the fetus, the maternal immune system is not functionally immunosuppressed and may be more responsive to systemic infections (16). More research is needed to clarify how the immune changes of pregnancy alter autoimmunity.
Pregnancy results in new exposures to alloantigens both at the level of the placenta and systemically as fetal DNA and small populations of fetal cells enter maternal circulation (microchimerism). Microchimerism may be critical for immune tolerance and may impact autoimmunity (17,18). Insufficient fetal microchimerism may increase inflammation with lower levels seen in women with preeclampsia (19). Improvement in rheumatoid arthritis during pregnancy has been correlated with higher levels of fetal microchimerism (20). However, fetal microchimerism may correlate with progressive disease in other autoimmune diseases like systemic lupus erythematosus and systemic sclerosis (21). Further investigation is needed to understand the impact of microchimersim on the maternal immune system particularly in light of persistence of fetal microchimerism in maternal circulation for years after pregnancy. It is unknown how microchimerism affects the risk and course of an autoimmune disease, like ITP.
Prenatal risks and management
ITP often worsens during the course of pregnancy with only 5.6% of women with ITP having improvement in platelet counts during pregnancy (2). The majority of women with pre-existing ITP have worsening thrombocytopenia during pregnancy and nearly half (49%) require treatment (2). Risk factors for severe disease during pregnancy include prior splenectomy, as well as a short duration of response to IVIG and/or inability to taper glucocorticoids (3). Rapidly declining platelet counts suggests worsening ITP: these mothers require closer monitoring than those with stably low counts.
The decision to start therapy is based on the degree of thrombocytopenia, signs of bleeding, and status of the pregnancy. During the first and second trimesters, platelet counts may be safely maintained at 20
First line therapies are similar to ITP in the non-pregnant patient. IVIG and glucocorticoids appear to have similar efficacy in peripartum ITP and have minimal risk to the fetus (22). Glucocorticoids should be tapered to the lowest possible dose; higher doses of glucocorticoids (especially >15 mg/day) can increase the risk of maternal diabetes, hypertension and excessive weight gain and the risk of an abnormal fetal weight (23). IVIG is considered safe in pregnancy, however the prothrombotic risk of IVIG is notable given the already increased risk for thrombosis in pregnancy (24). Patients with a shorter duration of response to IVIG may benefit from more frequent dosing such as lower doses given biweekly (3). Combination therapy with both glucocorticoids and IVIG may be effective in women who have insufficient platelet count responses to either treatment as monotherapy. If combination therapy is ineffective, second line therapies should be considered.
Second line treatment choices must take in to account the expected timing of response and the course of pregnancy. Some second line therapies require months for a response. Cyclosporine, for example, will only be effective by delivery if considered earlier in pregnancy. In emergencies with an urgent need to increase the platelet count, IVIG with or without high dose steroids is recommended. Platelet transfusions may also be helpful. The risk of antifibrinolytic therapies during pregnancy is unknown although it is safe and effective for postpartum bleeding (25).
Additionally, the impact on maternal and fetal outcomes must be considered when selecting second line therapies. Anti-D immune globulin (Winrho®) has been used for RhD-positive women with ITP during the second and third trimesters, however there is a risk of both maternal and fetal hemolysis (depending on the fetus’s RhD status) (26). Rituximab may be considered, but may cause neonatal lymphopenia and impaired response to vaccinations (27). Azathioprine has been used successfully in pregnancy with more extensive data on the use in systemic lupus erythematosus and renal transplantation (28). Splenectomy should be avoided except in the most treatment refractory settings (3,29). If needed, it is preferred to perform a splenectomy during the second trimester when there is the least risk to the fetus from anesthesia and uterine size is not prohibitive (30). Notably, vaccinations against encapsulated organisms will be required and splenectomy will increase the mother’s risk for thrombosis (31). Contraindicated ITP directed therapies due to adverse fetal outcomes include: syk inhibitors, vinca alkaloids, mycophenolate mofetil, cyclophosphamide and danazol (3).
Data is emerging on the safety of TPO-RAs and pregnancy. Pregnant women were excluded from the trials of romiplostim and eltrombopag and minimal long term safety data is available on fetal outcomes. Both romiplostim and eltrombopag likely cross the placenta as romiplostim utilizes the fc receptor and eltrombopag is a small molecule. The majority of women with ITP in pregnancy respond to the TPORAs with one case series showing a 77% response rate although most responders (70%) required multiple concurrent ITP therapies (32). Romiplostim appears safe in pregnancy based on a limited safety database from the manufacturer and other case series (3,32). Romiplostim may be preferred over eltrombopag due to the lack of iron chelation and liver toxicity (33). However, the liver effects of eltrombopag may be overreported in the general literature due to the interference effects of eltrombopag on laboratory testing (33). A small case series reported no adverse effects of eltrombopag in pregnancy except for one neonate with thrombocytosis that persisted for weeks after delivery with a mother who continued to take eltrombopag while breastfeeding (32). Human recombinant TPO (rhTPO) has also been successfully used in pregnancy in one case series (34), but is not universally available.
Delivery risks and management
Coordination with each patient and her obstetrician is essential throughout pregnancy but especially close to delivery. ITP can worsen in the third trimester and close monitoring is required especially for women with a rapidly falling platelet count. The route of delivery is based on pregnancy indications (35). Ideally, platelet counts should be above 50×109/L prior to vaginal delivery as the risk of postpartum hemorrhage increases below 50×109/L (2). If a mother desires an epidural or will have an epidural a cesarean delivery, a platelet count above 70×109/L is recommended (3). In a series of thrombocytopenic patients, the risk of bleeding with an epidural was 0.2% when the platelet count was above 70×109/L (36). For a spinal block injection, a platelet count of 50×109/L is considered safe (37). If a mother requires an emergency cesarean, general anesthesia can be safely performed with a platelet count over 30×109/L (3,7). Postpartum pain control can include NSAIDs unless the platelet count is under 70×109/L (3,7). Women with ITP remain at risk for venous thrombosis (38) and prophylaxis should be used as indicated in routine pregnancy.
ITP can worsen after delivery, especially in women with a history of a splenectomy (2), and all should be closely monitored for postpartum hemorrhage. The incidence of postpartum hemorrhage varies by case series from 1.9% to 22% (6) with rates up to 24% in women with platelet counts under 50×109/L (6). The majority of women with ITP do not have bleeding complications beyond what is expected during pregnancy as the most important mechanism of hemostasis after delivery is the normal contraction of the uterus after delivery
Risks for the neonate and management
After delivery, close monitoring of the neonate is required as 21% to 28% will develop thrombocytopenia presumably from passive transfer of maternal autoantibodies against platelet antigens (6). The majority have mild thrombocytopenia without life threatening bleeding. Less than 1% of neonates develop intracranial hemorrhage (3,39). Risk for thrombocytopenia is increased if siblings had thrombocytopenia at delivery or if the mother has had a splenectomy (39). Except for one retrospective case series (40), most data suggest the mother’s treatment and platelet counts during pregnancy do not impact the risk of thrombocytopenia in the neonate (32,39). Attempts to measure the fetal platelet count by percutaneous umbilical blood sampling is not recommended as there is a risk of hemorrhage and fetal loss comparable to non-intervention (Table 1). Fetal scalp vein sampling also has a risk of hemorrhage and may result in a falsely low platelet count.
Although most infants are unaffected, it is critical to avoid trauma to the infant during delivery and the use of forceps or vacuum should be discouraged. After birth, a cord blood platelet count should be sent. If this is less than 100×109/L, a peripheral blood platelet count should be drawn and followed until the platelet count stabilizes above 100×109/L. Pseudothrombocytopenia should be excluded as it is common with cord blood draws due to a higher rate of clotting in the sample (3). Platelet counts may decline during the first 1–3 days of life (3). Treatment with IVIG is indicated if the infant has signs of bleeding and/or a platelet count under 30×109/L (3,7). If there is an intracranial hemorrhage, the platelet count should be kept above 100×109/L for one week and then above 50×109/L in the second week (3). Platelet transfusions may also be used although they may increase the risk of intracranial hemorrhage if used when the platelet count is at or above 50×109/L (33).
Breastfeeding and ITP
The majority of women with ITP may breastfeed if desired. Rarely, breastfeeding may cause persistent neonatal thrombocytopenia that resolves when breastfeeding is stopped (3,39). If there is persistent neonatal thrombocytopenia, breastfeeding should be discontinued. If the mother would like to resume breastfeeding after the baby’s platelet count recovers, then the mother should be advised to express breast milk to maintain her ability to breastfeed. Breastfeeding may be resumed if the baby’s platelet count improves and remains stable once restarted. The mother’s ITP treatment may also impact counseling around breastfeeding as some medications are secreted in breast milk such as glucocorticoids (41). Eltrombopag may also be secreted in breastmilk as persistent thrombocytopenia after birth was noted in one infant whose mother breastfed while on eltrombopag (32).
Conclusions
ITP can be successfully managed in the peripartum setting with close monitoring and coordination with obstetrics and pediatrics. Although mothers are at risk for worsening ITP as pregnancy progresses and nearly half require treatment, ITP is not a contraindication for pregnancy. Frontline therapy consists of glucocorticoids or IVIG. Combination therapy can be used if there is an inadequate response to frontline therapies. Second line therapies can be successful, but require discussion with the mother regarding potential risks to herself and her baby. Limited case series suggest the TPORAs and rhTPO are safe in pregnancy. Additional investigation is needed to understand the impact of immune modulation of pregnancy on the development and severity of ITP in the peripartum setting.
Acknowledgments
Funding: Dr. Poston received a 2019 HTRS/Novo Nordisk Clinical Fellowship Award in Hemophilia and Rare Bleeding Disorders from the Hemostasis and Thrombosis Research Society (HTRS), which was supported by an educational grant from Novo Nordisk Inc.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (John W. Semple and Rick Kapur) for the series “Treatment of Immune Thrombocytopenia (ITP)” published in Annals of Blood. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aob-20-58). The series “Treatment of Immune Thrombocytopenia (ITP)” was commissioned by the editorial office without any funding or sponsorship. JNP reports grants from Novo Nordisk/HTRS, outside the submitted work. TBG reports personal fees from Amgen Corporation, personal fees from Novartis Corporation, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Care A, Pavord S, Knight M, et al. Severe primary autoimmune thrombocytopenia in pregnancy: a national cohort study. BJOG 2018;125:604-12. [Crossref] [PubMed]
- Loustau V, Debouverie O, Canoui-Poitrine F, et al. Effect of pregnancy on the course of immune thrombocytopenia: a retrospective study of 118 pregnancies in 82 women. Br J Haematol 2014;166:929-35. [Crossref] [PubMed]
- Provan D, Arnold DM, Bussel JB, et al. Updated international consensus report on the investigation and management of primary immune thrombocytopenia. Blood Adv 2019;3:3780-817. [Crossref] [PubMed]
- Verdy E, Bessous V, Dreyfus M, et al. Longitudinal analysis of platelet count and volume in normal pregnancy. Thrombosis Haemostasis 1997;77:806-7. [Crossref] [PubMed]
- Reese JA, Peck JD, Deschamps DR, et al. Platelet Counts during Pregnancy. N Engl J Med 2018;379:32-43. [Crossref] [PubMed]
- Eslick R, McLintock C. Managing ITP and thrombocytopenia in pregnancy. Platelets 2020;31:300-6. [Crossref] [PubMed]
- Gernsheimer T, James AH, Stasi R. How I treat thrombocytopenia in pregnancy. Blood 2013;121:38-47. [Crossref] [PubMed]
- Ruggeri M, Schiavotto C, Castaman G, et al. Gestational thrombocytopenia: a prospective study. Haematologica 1997;82:341-2. [PubMed]
- Christensen RD, Henry E, Del Vecchio A. Thrombocytosis and thrombocytopenia in the NICU: incidence, mechanisms and treatments. J Matern neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet 2012;25 Suppl 4:15-7.
- Guo L, Kapur R, Aslam R, et al. CD20+ B-cell depletion therapy suppresses murine CD8+ T-cell-mediated immune thrombocytopenia. Blood 2016;127:735-8. [Crossref] [PubMed]
- Zhang X, Zhao Y, Li X, et al. Thrombopoietin: a potential diagnostic indicator of immune thrombocytopenia in pregnancy. Oncotarget 2016;7:7489-96. [Crossref] [PubMed]
- Makar RS, Zhukov OS, Sahud MA, et al. Thrombopoietin levels in patients with disorders of platelet production: diagnostic potential and utility in predicting response to TPO receptor agonists. Am J Hematol 2013;88:1041-4. [Crossref] [PubMed]
- Ferreira LMR, Meissner TB, Tilburgs T, et al. HLA-G: At the Interface of Maternal-Fetal Tolerance. Trends Immunol 2017;38:272-86. [Crossref] [PubMed]
- Hackmon R, Pinnaduwage L, Zhang J, et al. Definitive class I human leukocyte antigen expression in gestational placentation: HLA-F, HLA-E, HLA-C, and HLA-G in extravillous trophoblast invasion on placentation, pregnancy, and parturition. Am J Reprod Immunol 2017;77: [Crossref] [PubMed]
- Szekeres-Bartho J, Wegmann TG. A progesterone-dependent immunomodulatory protein alters the Th1/Th2 balance. J Reprod Immunol 1996;31:81-95. [Crossref] [PubMed]
- Witkin SS, Linhares IM, Bongiovanni AM, et al. Unique alterations in infection-induced immune activation during pregnancy. BJOG 2011;118:145-53. [Crossref] [PubMed]
- Mincheva-Nilsson L, Baranov V. Placenta-derived exosomes and syncytiotrophoblast microparticles and their role in human reproduction: immune modulation for pregnancy success. Am J Reprod Immunol 2014;72:440-57. [Crossref] [PubMed]
- Kinder JM, Stelzer IA, Arck PC, et al. Immunological implications of pregnancy-induced microchimerism. Nat Rev Immunol 2017;17:483-94. [Crossref] [PubMed]
- Hahn S, Hasler P, Vokalova L, et al. Feto-Maternal Microchimerism: The Pre-eclampsia Conundrum. Front Immunol 2019;10:659. [Crossref] [PubMed]
- Guthrie KA, Dugowson CE, Voigt LF, et al. Does pregnancy provide vaccine-like protection against rheumatoid arthritis? Arthritis Rheum 2010;62:1842-8. [Crossref] [PubMed]
- Adams Waldorf KM, Nelson JL. Autoimmune disease during pregnancy and the microchimerism legacy of pregnancy. Immunol Invest 2008;37:631-44. [Crossref] [PubMed]
- Sun D, Shehata N, Ye XY, et al. Corticosteroids compared with intravenous immunoglobulin for the treatment of immune thrombocytopenia in pregnancy. Blood 2016;128:1329-35. [Crossref] [PubMed]
- Bandoli G, Palmsten K, Forbess Smith CJ, et al. A Review of Systemic Corticosteroid Use in Pregnancy and the Risk of Select Pregnancy and Birth Outcomes. Rheum Dis Clin North Am 2017;43:489-502. [Crossref] [PubMed]
- Stiehm ER. Adverse effects of human immunoglobulin therapy. Transfus Med Rev 2013;27:171-8. [Crossref] [PubMed]
- . Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet 2017;389:2105-16. [Crossref] [PubMed]
- Michel M, Novoa MV, Bussel JB. Intravenous anti-D as a treatment for immune thrombocytopenic purpura (ITP) during pregnancy. Br J Haematol 2003;123:142-6. [Crossref] [PubMed]
- Chakravarty EF, Murray ER, Kelman A, et al. Pregnancy outcomes after maternal exposure to rituximab. Blood 2011;117:1499-506. [Crossref] [PubMed]
- Natekar A, Pupco A, Bozzo P, et al. Safety of azathioprine use during pregnancy. Can Fam Physician 2011;57:1401-2. [PubMed]
- Mahey R, Kaur SD, Chumber S, et al. Splenectomy during pregnancy: treatment of refractory immune thrombocytopenic purpura. BMJ Case Rep 2013;2013:bcr2013201778 [Crossref] [PubMed]
- Bleau N, Czuzoj-Shulman N, Spence AR, et al. Safety of splenectomy during pregnancy. J Matern Fetal Neonatal Med 2017;30:1671-5. [Crossref] [PubMed]
- Cadili A, de Gara C. Complications of splenectomy. Am J Med 2008;121:371-5. [Crossref] [PubMed]
- Michel M, Ruggeri M, Gonzalez-Lopez TJ, et al. Use of thrombopoietin receptor agonists for immune thrombocytopenia in pregnancy: results from a multicenter study. Blood 2020;136:3056-61. [Crossref] [PubMed]
- Vlachodimitropoulou E, Chen YL, Garbowski M, et al. Eltrombopag: a powerful chelator of cellular or extracellular iron(III) alone or combined with a second chelator. Blood 2017;130:1923-33. [Crossref] [PubMed]
- Kong Z, Qin P, Xiao S, et al. A novel recombinant human thrombopoietin therapy for the management of immune thrombocytopenia in pregnancy. Blood 2017;130:1097-103. [Crossref] [PubMed]
- . ACOG Practice Bulletin No 207: Thrombocytopenia in Pregnancy. Obstet Gynecol 2019;133:e181-93. [Crossref] [PubMed]
- Lee LO, Bateman BT, Kheterpal S, et al. Risk of Epidural Hematoma after Neuraxial Techniques in Thrombocytopenic Parturients: A Report from the Multicenter Perioperative Outcomes Group. Anesthesiology 2017;126:1053-63. [Crossref] [PubMed]
- Bauer ME, Arendt K, Beilin Y, et al. The Society for Obstetric Anesthesia and Perinatology Interdisciplinary Consensus Statement on Neuraxial Procedures in Obstetric Patients with Thrombocytopenia. Available online: https://soap.memberclicks.net/assets/docs/SOAP_Thrombocytopenia_Consensus_Statement_FINAL_STATEMENT.pdf
- Machin N, Ragni MV, Comer DM, et al. Prevalence and correlates of thrombosis in adults with immune thrombocytopenia: An NIS study. Thromb Res 2018;172:80-5. [Crossref] [PubMed]
- Payne SD, Resnik R, Moore TR, et al. Maternal characteristics and risk of severe neonatal thrombocytopenia and intracranial hemorrhage in pregnancies complicated by autoimmune thrombocytopenia. Am J Obstet Gynecol 1997;177:149-55. [Crossref] [PubMed]
- van der Lugt NM, van Kampen A, Walther FJ, et al. Outcome and management in neonatal thrombocytopenia due to maternal idiopathic thrombocytopenic purpura. Vox Sang 2013;105:236-43. [Crossref] [PubMed]
- Brooks PM, Needs CJ. The use of antirheumatic medication during pregnancy and in the puerperium. Rheum Dis Clin North Am 1989;15:789-806. [PubMed]
Cite this article as: Poston JN, Gernsheimer TB. Management of immune thrombocytopenia in pregnancy. Ann Blood 2021;6:5.