
Blood banking in solid organ transplantation
Introduction
Organ transplantation is now performed worldwide in over 80 countries. The Global Observatory on Donation and Transplantation (GODT), a collaboration of the World Health Organization and the Spanish Organización Nacional de Trasplantes, estimated that in the year 2019 there were 100,097 kidneys (+44% from their first report in 2008), 35,784 livers (+76%), 8,722 hearts (+64%), 6,800 single or double lungs (+104%), 2,323 pancreases (−2%) and 153,863 total organs transplanted (+52%) (1,2). On a per-capita basis, the top 5 countries in 2019 were the United States (US), Spain, France, Korea and Canada (83–123 transplants per million population). However, in absolute numbers the top 5 were the US [40,621], China [19,462], India [12,666], Brazil [9,232] and France [5,910], just ahead of Turkey [5,763]. In the US, 2020 totals kept pace with 2019 despite the COVID-19 pandemic (3).
Current one-year patient survivals in US data are 89–91% for heart, lung and pancreas transplants, 94% for livers, and 96–99% for deceased donor (DD) and living donor (LD) kidneys (Table 1). However, waitlists are 1 to 4 times the annual transplant totals for most organs. Waitlist mortality rates for lung, heart and liver candidates are 9–15% and 5% for DD kidney candidates. These statistics help illustrate the impetus to expand organ access, including ABO-incompatible (ABO-i) organs.
Table 1
| Parameters | Kidneys | Kidney-pancreas | Livers | Hearts | Lungs |
|---|---|---|---|---|---|
| LD | 5,234 | 0 | 491 | 0 | 0 |
| % LD | 23% | – | 6% | – | – |
| DD | 17,583 | 827 | 8,415 | 3,658 | 2,539 |
| Total in 2020 | 22,817 | 827 | 8,906 | 3,658 | 2,539 |
| 1 yr patient survival in 2019 | 96–99% | 97% | 94% | 91% | 90% |
| Waitlist on 9/30/21 | 97,806 | 1,855 | 11,982 | 3,540 | 1,014 |
| Ratio waitlist : 1 yr transplants | 4.3× | 2.2× | 1.3× | 1.0× | 0.4× |
| Waitlist mortality during 2019–2021 | 5% DD | 4% | 12% | 9% | 15% |
US Organ Procurement and Transplantation Network (OPTN) data, October 1, 2021 (3). Accessed at https://optn.transplant.hrsa.gov/data/. LD, living donor; DD, deceased donor.
Organ transplant patients require comprehensive transfusion medicine support throughout their full course, from evaluation of candidates with ABO typing and antibody titers to the treatment of rejection with therapeutic apheresis. The purposes of this narrative review are to summarize current knowledge of blood transfusion requirements, red blood cell (RBC) alloantibody problems, passenger lymphocyte antibodies, the laboratory support of ABO-i transplants including antibody titers, and therapeutic apheresis indications. Selected reviews in these areas are cited for more focused information.
Perioperative transfusions
Table 2 shows perioperative blood component usage in numerous liver transplant programs. The earliest data from Pittsburgh in 1981 is shown for historical comparison. The Nashville program demonstrated significant transfusion reductions by instituting transfusion guidelines, education, intraoperative RBC salvage and viscoelastometric testing (5). Their post-intervention usage and most of the other series were in the range of 4–8 mean or median intraoperative RBCs and a similar number of units of plasma. The 75th-percentile levels for RBCs ranged from 7–12 units. Intraoperative RBC salvage is commonly used, with 700 mL (mean) and 1,300 mL (median) transfused in Pittsburgh 2013–2014 and in Nashville’s intervention phase (5,7). Mean or median intraoperative platelet needs were 1 to 1.5 doses per case. The Toronto and Pittsburgh experiences are of interest because workers published two series at different times, and both programs tended to use less RBCs and plasma in later years (6-9). Table 3 and Table 4 show six studies which sought risk factors for higher blood use. Anemia, thrombocytopenia and elevated international normalized ratios or viscoelastometry clotting times were frequently cited, reinforcing the benefits of preoperative patient blood management measures to correct cytopenias and coagulopathies. The Detroit experience was useful because it included preoperative (−1 week) and postoperative (+2 weeks) transfusions in addition to intraoperative usage (12). Across this perioperative period, these patients received approximately twice as many units as in the surgery itself.
Table 2
| Location | Year | n | RBC | Plasma | Platelets | Theme |
|---|---|---|---|---|---|---|
| Pittsburgh (4) | 1981 | 17 | 36 (± NA) | 36 (± NA) | 5 (± NA) | Early experience |
| Nashville (5) | 2010–2011 | 156 | 14±17 | 16±16 | 1.5±2.3 | Before interventions |
| 2012–2013 | 125 | 7±9 | 11±12 | 1.1±1.4 | After interventions | |
| Pittsburgh (6) | 2004–2006 | 475 | 9 [4–11] | 7 [2–9] | 1.6 (0–2.4) | No pulmonary embolism |
| Pittsburgh (7) | 2013–2014 | 36 | 6 [3–9] | 4 [3–6] | 1 (0–2) | Hemostasis testing |
| Toronto (8) | 1998–2004 | 460 | 5 [3–9] | 9 [6–14] | 1 (0–2) | High-use prediction |
| Toronto (9) | 2002–2015 | 1,420 | 4 [1–7] | 6–8 [3–11] | 1–1.5 (0–5) | Tranexamic acid effect |
| Seattle (10) | 2013–2015 | 207 | 5±4 | NA | NA | High-use prediction |
| Baltimore (11) | 2014–2016 | 200 | 6 [2–12] | 7 [2–13] | NA | High-use prediction |
| Detroit (12) | 2007–2017 | 970 | 6±7 | 10±9 | 2.0±1.8 | Blood use |
| Melbourne (13) | 2009–2018 | 175 | 3 (0–6) | 0 (0–3) | 0 (0–2) | No donor blood, paired |
| 175 | 2 (0–4) | 1 (0–4) | 0 (0–2) | Deceased donor blood | ||
| Essen (14) | 2009–2010 | 266 | 2 (0–5) | 0 (0–0) | 0 (0–1) | Factor concentrates |
| Montreal (15) | 2002–2013 | 500 | 0.5±1.3 | 0.2±1.1 | 0.1±1.0 | Minimal transfusions |
| Los Angeles (16) | 1999–2004 | 27 | 0 | 0 | 0 | Jehovah’s Witnesses |
| Pisa (17) | 2007–2016 | 13 | 0 | 0 | 0 | Jehovah’s Witnesses |
| Scottsdale (18) | 2001–2004 | 69 DD | 2.9±2.7 | 2.5±2.4 | 1.2±1.0 | Compared to LD |
| 27 LD | 1.0±1.6 | 0.8±1.5 | 0.4±0.7 | Lower use in LD cases | ||
| Chengdu (19) | 2005–2012 | 218 LD | 7.9±6.6 | NA | NA | Blood use and outcomes |
| Cairo (20) | 2005–2015 | 123 LD | 9.5± (NA) | 9.1± (NA) | 2.9± (NA) | Blood use and outcomes |
| Bergamo (21) | 2002–2009 | 243 (children) | 1 (NA) | 1.6 (NA) | 0 (NA) | Blood use & outcomes |
| Paris (22) | 2009–2014 | 84 (children) | 0.6 BV (0–6) | NA | NA | High-use prediction |
| Pittsburgh (23) | 2008–2017 | 278 (children) | 0.2 BV (0–0.5) | NA | NA | High-use factors |
Mean ± standard deviation (SD) or median (interquartile range). Transfusions were all intraoperative (IO) except IO plus 24 hr in Toronto. Pittsburgh 2004–2006 series was compared to 20 other patients with pulmonary embolism. Cairo transfusion means were calculated from their data in two groups. Platelets are expressed in apheresis units or pools (5 whole-blood derived units per pool if not specified). RBC, red blood cell; BV, blood volume; DD, deceased donor; LD, living donor; NA, not available.
Table 3
| Risk factor | Toronto (8) | Seattle (10) | Baltimore (11) |
|---|---|---|---|
| High use definition | ≥6 U in 24 hr | >1.25 L & >2 L RBC IO | >10 U IO |
| Risk expression | Points | On–line calculator | Points |
| Patient factors | Age >40; Retransplant | Dialysis; Past spontaneous bacterial peritonitis | Liver-kidney transplant; Retransplant |
| Hematology tests | Hgb <10 g/dL; Platelets ≤70,000/μL; INR 1.2–2 or >2 | Hgb; INR | Hgb <10 g/dL; Platelets <100,000/μL; TEG R >6 min |
| Other tests | Albumin ≤24 g/L; Cr >110 (F) or >120 (M) mmol/mL |
RBC, red blood cell; Cr, creatinine; F, female; Hgb, hemoglobin; INR, international normalized ratio; M, male; IO, intraoperative; TEG R, thromboelastography R value; U, units.
Table 4
| Risk factor | Paris (18) | Boston (24) | Houston (25) |
|---|---|---|---|
| High use definition | >1 BV RBCs IO | >1 BV loss in 24 hr | >85th percentile blood use |
| Risk expression | Points | List | List |
| Patient factors | Ex situ liver transection Prior abdominal surgery | In hospital; split or reduced-sized graft | |
| Hematology tests | Factor V ≤30% | Hgb <8.5 g/dL; platelets <100,000/μL | |
| Surgical | Surgery >10 hr | Operative time; use of plasma, cryoprecipitate |
RBC, red blood cell; BV, blood volume; IO, intraoperative.
In North America and Europe, LD for adult livers are in the minority (6% in the US, Table 1), usually selectively arranged for patients with less advanced disease and lower DD priority scores. In this scenario blood needs in LD transplants may be significantly lower, as seen in Scottsdale (18). However, in other regions such as the Middle East, DD are infrequent, LD are used routinely, and blood usage such as in Chengdu and Cairo may be similar to routine DD cases elsewhere (19,20). In a large multicenter analysis, only 2% of 5,202 living liver donors needed RBC transfusions (26).
Melbourne’s program described collecting blood from DDs for recipients (13). In donors who were ABO-matched, RhD-compatible, and cytomegalovirus (CMV)-status-compatible (avoiding CMV+ to CMV−), a RBC salvage reservoir full of heparinized donor blood (4 units) was retrieved with the liver, crossmatched with the recipient, washed and processed in the operating room cell salvage instrument, and transfused as needed. Patients receiving donor blood (median 3 units) used less intraoperative blood bank RBCs than propensity-matched patients who did not have donor blood available.
“Dead-icated” deceased blood donors and organ transplants have intersected before. The curious reader may consult Ramsey and Schmidt’s historical essay for information about how cadaver blood collections in the Soviet Union in the 1930s–1960s were inspired by the first kidney transplants there (27). That experience led a surgeon at a small Chicago-area hospital to secretly give cadaver blood transfusions in the 1930s, before one of his colleagues at the same facility later performed the first briefly functional DD kidney transplant in Western medicine in 1950.
Four liver transplant series were notable because of their unusually low transfusion needs. Kirchner et al. replaced plasma for clotting factors with factor concentrates and fibrinogen concentrate and gave very few units of plasma and platelets (14). Massicotte et al. described 500 liver transplants in Montreal which averaged 0.5 units of RBCs and <0.2 units of plasma and platelets intraoperatively (15). Eighty percent received no RBCs. They performed surgery with low central venous pressures, minimum volume replacement and avoidance of plasma and platelets until bleeding occurred. Jabbour et al. and Costanzo et al. described bloodless management in two cohorts of Jehovah’s Witnesses in the US and Italy who did not permit transfusions (16,17).
Table 2 shows blood use information in pediatric liver transplants. Three series with transfusion data had different patient populations, judging from the patient ages. Younger patients received proportionally higher RBCs/blood volume. These and other studies examined preoperative risk factors for higher blood use, and split livers used more blood in two studies (Tables 3,4). The Bergamo group found that patients receiving ≥3 RBC or plasma units intraoperatively (compared to medians of 1 and 1.6 U) had lower 1-year patient survivals (21).
Table 5 tabulates recent data on transfusions in heart transplants. Programs in Pittsburgh and Newcastle had median or mean transfusions of around 3 RBCs, 2–4 plasma units and 1 platelet unit. These studies found correlations between higher transfusions and increased postoperative complications such as graft dysfunction. Several centers including ours described introduction of 4-factor concentrates to reverse warfarin before surgery, showing not only reduced plasma usage but also sometimes reduced RBC transfusions. Transfusions in the 4-factor-concentrate patient groups were similar to the above numbers.
Table 5
| Location | Years | n | Interval | RBC | Plasma | Platelets | Theme |
|---|---|---|---|---|---|---|---|
| All UK (28) | 2012–2015 | 450 | IO? | 2.7 | 2 | 1.4 | PGD & transfusions |
| No PGD | 287 | 2 | 2 | 1 | |||
| PGD | 163 | 4 | 2 | 2 | |||
| Pittsburgh (29) | 2010–2016 | 197 | IO + 24 hr | 3 [1–5] | 4 [1–8] | 1 (0–2) | Transfusions & adverse events |
| Norfolk US (30) | 2011–2015 | 12 | IO + 24 hr | 7 | 8 | 2.5 | Warfarin-plasma |
| 13 | 3 | 4 | 2 | Warfarin-4FC | |||
| Chicago (31) | 2010–2015 | 39 | IO | 7 [4–9] | 9 [6–13] | 4 [2–6] | Warfarin-plasma |
| 21 | 3 [1–5] | 4 [1–6] | 4 [2–4] | Warfarin-4FC | |||
| Cleveland (32) | 2010–2016 | 49 | Day 0–2 | 6 [3–9] | 8 [6–10] | 2 [2–3] | Warfarin-plasma |
| 57 | 7 [4–11] | 6 [4–8] | 2 [1–3] | Warfarin-4FC | |||
| Boston (33) | 2013–2016 | 42 | IO | 5 [3–7] | 6 [4–8] | 2 (1.5–2.5) | Warfarin-plasma |
| 32 | 2 [1–3] | 1 (0–2) | 2 (1.5–2.5) | Warfarin-4FC | |||
| Newcastle (34,35) | 2003–2013 | 311 (lung) | 24 hr | 3 (NA) | 2 (NA) | 1 (NA) | Transfusions & outcomes |
| Brisbane (36) | 2010–2014 | 47 (lung) | IO | 4.4 | 3.6 | 1.4 | Before POC testing |
| 46 (lung) | 1.6 | 0.1 | 0.2 | POC testing | |||
| Prague (37) | 2018–2020 | 36 (lung) | IO + 24 hr | 3.1 | 7.8 | 0.6 | Before ROTEM |
| 31 (lung) | 1.7 | 0 | 0.2 | ROTEM | |||
| Multiple (38) | 2020 | 12 (lung) | IO | 8 [5–15] | 4 [3–7] | NA | COVID-19 transplants |
Mean ± SD or median (IQR). RBC, red blood cell; 4FC, 4-factor concentrate; BV, blood volume; IO, intraoperative; N, number; NA, not available; POC, point of care; PGD, primary graft dysfunction; ROTEM, rotational thromboelastometry; US, United States.
Table 5 displays data on blood use in lung transplants. The Newcastle program gave intraoperative medians of 3 RBCs, 2 plasmas and 1 platelet unit. Studies from Brisbane and Prague showed that intraoperative hemostasis testing reduced intraoperative and postoperative blood needs. Their average intraoperative transfusions guided by testing were around 2 RBCs and ≤0.2 units of plasma and platelets. These were all in bilateral lung transplants. Huddleston et al. did not report overall RBC usage, but from their Table 1 we calculated that 44% of single-lung patients received intraoperative RBCs compared to 87% of bilateral lung transplants (39). Initial experience at our institution and elsewhere with lung transplants in COVID-19 patients has seen higher intraoperative blood use due to dense pleural adhesions, with medians [interquartile ranges] of 8 [5–15] RBCs and 4 [3–7] plasma units (38).
Several lung transplant programs have correlated above-average transfusions with adverse outcomes in multivariate analyses controlling for other factors. In Newcastle, patients receiving >1 unit of platelets had decreased 1-year (but not 10-year) survival (34,35). In Minneapolis, patients receiving >15 units of RBCs had lower hazard-adjusted 30-day survival (39). In Durham, Seay et al. examined plasma:RBC ratios in patients receiving >4 units of RBCs in 72 hr, and when plasma units were >50% of RBC units, there was a higher rate of primary graft dysfunction (40). They instituted viscoelastometric testing late in their study period, so did not examine that impact on their findings.
Transfusions to lung donors might also adversely affect outcomes. This was examined in all US lung transplants from 1996 to 2014 (41). For the 6% of donors who received >10 units of RBCs, 30- and 90-day recipient multivariable-adjusted mortalities were 50% higher (approximately 6% vs. 4% at 30 days). This was linked to primary graft dysfunction, which has clinical similarities to transfusion-associated acute lung injury (TRALI), and the authors and the accompanying editorial speculated whether TRALI in donors might have contributed to these findings (41,42). During the latter part of this 18-year period, TRALI rates in the US declined substantially due to introduction of male-predominant plasma [2007] and human leukocyte antigen (HLA) antibody screening in parous plateletpheresis donors [2008–2009] (43). This decline leveled off after 2010 in the New York Blood Center’s timeline analysis, but the AABB standard for apheresis platelet screening did not take effect until 2016. The donor-transfusion study compared eras and the 2010–2014 era was not statistically different from earlier years, but this question could be reexamined in the current framework of TRALI mitigation. Current policies from the US Organ Procurement and Transplantation Network (OPTN) for organ donors do not require information on donor transfusions other than for assessment of hemodilution of infectious-disease test specimens (44).
Intraoperative blood transfusion needs for kidney or pancreas transplants have not been studied in recent years, but are generally modest. The blood order schedule at Johns Hopkins Hospital recommends 2 RBCs crossmatched for kidney and kidney-pancreas transplants (45).
Special blood component needs
Ex situ machine perfusion of donor lungs, livers and kidneys is increasingly employed and often includes blood bank RBCs in oxygenated circuits. Callaghan et al. reviewed several issues for this practice with regard to blood group compatibility, unit disposition tracing and potential infection transmission (46).
Leukoreduced RBC and platelet transfusions were formerly a special requirement in most organ transplant candidates and patients for mitigation of HLA alloimmunization and CMV exposure, but near-universal leukoreduction is now standard in most countries performing organ transplants.
Leukoreduction also appears to reduce the risk of transfusion-associated graft-versus-host disease (TA-GVHD) in patients in risk groups who inadvertently received unirradiated blood, but irradiation is still the standard of practice when indicated (47). TA-GVHD has been reported in 5 organ transplant patients, as reviewed by O’Brien et al. when describing the most recent case in 2013 (48). In a 2014 US practice survey of over 2,000 laboratories, a significant minority (37%) irradiated blood for solid organ transplants (49). However, given the rarity of these events when most patients receive unirradiated blood, most published recommendations and guidelines do not include all organ transplants (50,51).
The manufacturer of alemtuzumab (anti-CD52), used widely in organ transplant immunosuppression protocols, recommended blood irradiation in patients receiving the drug as CAMPATH for chronic lymphocytic leukemia (CLL) (52). The same manufacturer’s prescribing information for alemtuzumab as Lemtrada in smaller annual doses for multiple sclerosis does not recommend blood irradiation (53). In the 2014 survey, 29% irradiated blood for alemtuzumab recipients (49). In a 2015 review of TA-GVHD, all 3 author institutions irradiated blood for alemtuzumab patients (54).
The immunosuppressive risk from alemtuzumab for TA-GVHD was reexamined by Hui et al. in London (55). The drug manufacturer based their irradiation recommendation on one trial patient with CLL who had also received fludarabine, another drug with more established TA-GVHD risk. No other cases have been published. Hui et al. reviewed 647 renal transplant patients in their program who received alemtuzumab and were transfused with non-irradiated leukoreduced blood. No cases of TA-GVHD occurred. Based in part on these data, the British Society for Haematology removed alemtuzumab from their 2020 recommendations for blood irradiation (56).
RBC alloantibodies
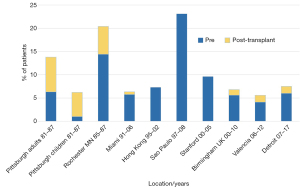
Most RBC antibody information in organ transplants comes from liver transplants, in which blood bank support is most affected. Figure 1 shows fairly constant RBC alloantibody rates in 10 cohorts of liver transplant patients over 30+ years. The preoperative median rate was 6.15% and the overall total median rate was 7.4%, with most series between 4–9%. The 1980s series had higher rates of postoperative antibodies, likely attributable to the higher blood use in that era. However, the overall rates have not changed over the entire period. In the series with gender information, male rates were 4–11% and female rates were 8–15%, and in individual series the female rates were 1.3 to 3 times the male rates. In adults this difference has been attributed to pregnancies, but even the Pittsburgh pediatric series showed the same trend, 4% in males and 8% in females (57).
We have examined the available data in these series for prevalence of difficult antibodies, defined as >3 antibodies or with <25% of donors antigen-negative, and 1–4% of all patients fit this criterion. When sufficient antigen-negative units may not be available, we have attempted to start with at least 10 compatible units, and as many more as possible, before switching to antigen-positive or antigen-untested units after some degree of antibody washout (65). We also take into account whether the antibody is currently detectable, although with some extra caution with historic Kidd antibodies. Clinicians are alerted to the possibility of a delayed hemolytic transfusion reaction. This approach generally has been successful for avoiding intraoperative hemolysis.
Antibodies to high-prevalence antigens pose special challenges when large numbers of RBCs may be needed. Case reports have described management of anti-PP1Pk, anti-Jra and anti-Jk3 in liver and heart transplants (66-68). One liver transplant patient with anti-e received e+ RBCs in surgery and then a postoperative RBC exchange with e-negative RBCs when they became available (69).
In most RhD-negative patients receiving RhD+ RBCs, the general anti-D alloimmunization rate is 20–35% (70). However, we and others have documented that the immunosuppression administered in organ transplantation appears to significantly reduce new anti-D formation (71-73). This allows for switching to RhD+ RBCs if the RhD− negative RBC supply is low. We are still cautious in girls and women of child-bearing age.
Passenger lymphocyte syndrome
In the 1980s we and many others recognized that kidney (74) and liver (75) transplants, especially from ABO-unmatched grafts such as O donors to non-O recipients, sometimes produced RBC antibodies as a humoral graft-versus-host response. The term ‘passenger lymphocyte syndrome’ (PLS) was adopted for this phenomenon (74). Although these antibodies were usually short-lived, there were cases of severe and rarely fatal hemolysis. We reviewed the burgeoning literature in 1991 (76). In ABO-unmatched transplants, ABO-antibody and hemolysis frequencies were 40% and 29% for livers and 17% and 9% for kidneys, respectively. By then we and others also began to encounter cases of non-ABO RBC antibodies, usually from donors whose antibody screens were positive prior to organ donation (77).
In the 30 years since our first review, this literature has continued to grow and other examples of antibody transfer beyond blood groups have been recognized. Table 6 shows key references for ABO PLS in more recent years, including several detailed reviews. For ABO, the authors of the post-1990 liver and kidney series mostly sought hemolysis, so their frequencies were more akin to hemolysis rates than to overall antibody rates. In 7 liver series since 1991, the aggregate hemolysis rate was 19%, and in three kidney series, the aggregate hemolysis rate was 6%. Both were somewhat lower than the 1980s experience of 29% and 9%, respectively. Thomas et al. recently reported a 12-year experience with ABO-unmatched intestinal and intestine-containing multivisceral transplants; 9 of 31 patients (29%) had PLS hemolysis (92). They also reviewed 7 previously reported intestinal cases. Presumably the larger lymphoid burden in intestinal transplants makes PLS more likely. Additional cases from lung and heart transplants were reported by Aujayeb et al. (91). In many centers, ABO-unmatched deceased-donor transplants are uncommon because of the need to provide group O patients with group O grafts. In the US in 2013–2015, 6% of DD adult liver transplants were ABO-unmatched, about 265 per year (93). Only 12% of these were O-to-A, the combination with the highest rate of hemolysis in our 1991 review. However, living-donor kidneys and liver segments are frequently ABO-unmatched with potential for PLS.
Table 6
| Organ | Reference | N or rate of hemolysis |
|---|---|---|
| Reviews | ||
| Kidney | Nadarajah 2013, (78) | |
| Liver | Romero 2015, (79) | |
| All 2009–2019 | Moosavi 2020, (80) | |
| Liver | Ramsey 1991 review, (76) | 33/115, 29% hemolysis; 36/90 with anti-A/B, 40% |
| Triulzi 1992, (81) | 5/9 | |
| Kunimasa 1998, (82) | 1/27 | |
| Romero 2015, (79) | 10/56 | |
| ElAnsary 2015, (83) | 2/11 | |
| De Bruijn 2017, (84) | 4/10 | |
| Woolfson 2019, (85) | 7/51 (pediatric) | |
| Brunetta 2020, (86) | 5/16 | |
| Sum post 1991 | 34/180, 19% hemolysis | |
| Kidney | Ramsey 1991 review, (76) | 15/165, 9% hemolysis; 24/144 with anti-A/B, 17% |
| Povlsen 1990, (87) | 0/108 Aza, 2/34 CsA | |
| Elhence 1998, (88) | 2/15 | |
| Bakr 2009, (89) | 10/214 | |
| Achkar 2011, (90) | 5/37 | |
| Sum post 1991 | 17/266, 6% hemolysis | |
| Lung | Aujayeb 2014, (91) | 6 cases |
| Heart | Aujayeb 2014, (91) | 1 case |
| Intestine-containing | Thomas 2021, (92) | 9/31, 29% hemolysis |
Aza, azathioprine; CsA, cyclosporin A.
Anti-D was transferred in >30 cases (Table 7). In a series of 97 lung transplants in Toronto, the only two donors with anti-D both transferred the antibodies to their 3 recipients (100). Other donor-derived RBC antibodies in the Rh, Kell, Kidd, Duffy and MNS blood groups have been seen. The US OPTN does not require determination of donor RBC antibody status, and transfusion services usually do not know who will become a deceased organ donor. However, when organ donors are found to have RBC antibodies, it seems prudent to notify the transplant service and type the recipient’s RBCs for the cognate antigens so that potential PLS can be anticipated.
Table 7
| Antibody & organ | Reference | Cases & antibodies |
|---|---|---|
| Reviews | ||
| Anti-D | Ainsworth 2009, (94) | 23 cases reviewed |
| Non-ABO RBC | Draper 2018, (95) | |
| Anti-D since 2009 | ||
| Liver | Turiño-Luque 2012, (96) | 1 |
| ElAnsary 2015, (83) | 1 | |
| Romero 2015, (79) | 2 | |
| Gniadek 2017, (97) | 1 | |
| Tsang 2019, (98) | 1 | |
| Kidney | Karanth 2014, (99) | 1 |
| Kidney-pancreas | Tsang 2019, (98) | 1 |
| Lung | Cserti-Gazdewich 2009, (100) | 3 |
| Other RBC antibodies | ||
| Liver | Kim 1992, (101) | D-E |
| Seltsam 2001, (102) | K-Fya | |
| Hareunevi 2002, (103) | Jka | |
| Grosskreutz 2008, (104) | D-C | |
| Shortt 2008, (105) | D-C-k | |
| De Luna 2011, (106) | E | |
| Koepsell 2013, (107) | Auto–anti-Kpb (donor +) | |
| Draper 2018, (95) | D-C | |
| Tsang 2019, (98) | Jka | |
| Kidney | Ramsey 1991 review, (76) | c [n=3], e |
| Schwartz 1992, (108) | D-C | |
| Larrea 1997, (109) | E | |
| ElAnsary 2015, (83) | C (and B) | |
| Kidney-pancreas | Seltsam 2001, (102) | K-Fya |
| Hurtarte-Sandoval 2015, (110) | D-E | |
| Multi-visceral | Makuria 2009, (111) | M |
RBC, red blood cell.
PLS antibodies typically develop 7–14 days after transplant and persist for a few weeks. Management usually consists of giving antigen-negative RBC transfusions. In severe PLS after intestinal transplantation, plasmapheresis and rituximab were employed (92). One liver transplant with anti-D was associated with profound reticulocytopenia (97).
Our 1991 review noted the first case of organ-transmitted immune thrombocytopenic purpura (ITP) (112) and speculated that transfer of other antibodies such as anti-CMV and anti-hepatitis C virus (HCV) was possible. Now to date, 7 cases of platelet autoantibody transfer (donor ITP) reviewed by Aranda Escaño et al. (113) and 6 cases of platelet alloantibody PLS (donor human platelet antigen antibodies) reviewed by French et al. (114), including one from our institution (115), have been reported (Table 8). There are also suspected cases of anti-HCV, anti-CMV and anti-HLA antibody transfers. One patient received factor VIII inhibitor antibody from a liver transplant (116).
Table 8
| Antibody | Reference | Cases |
|---|---|---|
| Platelet autoantibodies (ITP) | Aranda Escaño 2020, (113) | 7 cases reviewed |
| Platelet alloantibodies (HPA) | French 2020, (114) | 6 cases reviewed |
| Factor VIII inhibitor | Hisatake 2003, (116) | Liver recipient |
| HLA alloantibodies | Maxfield 2015, (117) | Donor -> 2 kidneys |
| HLA alloantibodies | Kummrow 2019, (118) | Donor -> 5 organs |
| Anti-CMV | Koshizuka 2019, (119) | Lung recipient |
| Anti-HCV | Smibert 2018, (120) | 4 lung recipients |
| IgE allergy transfer | Muller 2020 review, (121) | 10 cases; 7/9 donors died of anaphylaxis |
RBC, red blood cell; CMV, cytomegalovirus; HPA, human platelet antigens; HCV, hepatitis C virus; ITP, Immune thrombocytopenia.
PLS involves mostly but not exclusively IgG antibodies. Muller et al. recently reviewed 9 patients with IgE allergy transfer by organ transplants and investigated their own recipients of 3 donors who had died from anaphylaxis (121). One of their 3 donors transferred symptomatic peanut allergy to liver and lung recipients. In the 8 prior reports, 6 donors had died from anaphylaxis, and allergic reactions were acquired in liver, pancreas and lung (but not kidney) recipients. Two of the 3 lung transplant transfers were especially long-lasting, with persistence of peanut allergy for 1.5 to 7 years. The authors recommended that recipients of lungs, livers and pancreases from fatally anaphylactic donors should have allergy evaluations and avoid known inciting antigens until cleared by testing and monitored challenges. These cases illustrate that the production of probably any clinically significant donor antibody can be transferred to organ transplant patients in a conducive setting.
ABO incompatibility
ABO compatibility is normally required for organ transplants to avoid ABO-antibody-mediated acute rejection. Transplant recipient candidates and organ donors should have two independent typings to confirm their ABO blood group for listing and matching (44). The US OPTN published a guidance for blood type determination, summarizing for the transplant community familiar blood bank issues such as recent transfusions, allogeneic stem cell transplants, weak subgroups, acquired B-like antigens, and low ABO antibody levels (122). This document also discusses the ancillary use of DNA-based ABO phenotype prediction to assist with ambiguous typings caused by subgroups or massive transfusions. ABO genotyping test kits are not approved by the US Food and Drug Administration (FDA) but are available on a research-use-only basis employing technologies familiar to laboratories doing HLA typing. A Chinese group recently published their experience using ABO genotyping to resolve serologic typing discrepancies in 302 uremic patients with ABO subgroups (123). Although little to date has been published on ABO genotyping in organ donors, we can expect this area to grow.
As with blood transfusion, US OPTN policies require careful double-checking of correct and compatible organ and patient. A two-step process of preliminary and final time-out verification in the operating room is mandated before transplant. At our hospital the transfusion service enters each organ and its identification data into the laboratory information system as a “component”, performs an electronic ABO crossmatch with the recipient, and issues a compatibility tag similar to a transfusion tag to the operating room for their time-out verifications (124). Since 2004, we have processed >7,000 organ transplants without ABO error using this procedure.
Evasion of the ABO barrier to expand organ availability has been pursued in two ways: (I) weak A subgroup organs to B or O patients, and (II) fully ABO-i transplants. These comprise a small fraction of all transplants, but the transfusion medicine support of these protocols is a significant aspect of laboratory testing and therapeutic apheresis at the centers performing them. Kidney paired donations, in which donor-recipient pairs swap donors for compatibility purposes, can help avoid fully ABO-i transplants but may include A subgroup donors.
Around 20% percent of European or African-ancestry group A or AB persons’ RBCs are negative for the wild-type full-strength A1 antigen as determined by Dolichus biflorus A1 lectin (125). Most A1-negative subjects have the A2 genotype and express about 20% of the A1 level of antigens on their RBCs and endothelium. Group A or AB A1-negative organs (termed non-A1 in OPTN policies), mainly kidneys, can be transplanted to B or O persons with reasonably equivalent success rates, as discussed below. In US OPTN policies for DDs, A1 typing on two different specimens is required to confirm A1-negative status in group A donors and is optional in AB donors, when not precluded by recent transfusions. Patients can be listed as candidates for A1-negative organs if appropriate. A1-negative phenotypes are much less common in Asia (123,126). In east Asia, weak B subgroups presenting with plasma anti-B discrepancies and characterized with ABO genotyping (123) may be a future area of organ transplant investigation.
Correct donor A subgroup typing is crucial for safely and effectively allocating A and AB kidneys with A subgroups (Asub and AsubB). Recently the US-based College of American Pathologists (CAP) ABO subgroup proficiency testing program analyzed its results (127). A1 and A1B specimens were mistyped as A1-negative in 0.8% of results, which in real life could lead to inadvertent transplantation of A1-incompatible organs, if not caught by second typings. Nearly 5% of Asub challenges were mistyped as A1, which could lead to missed opportunities for A1-negative transplants.
Beginning in 2014, group B renal candidates in the US were accorded preferential allocation of A2 and A2B kidneys. In the first 2 years of this protocol, 9% of group B patients (150/year) received A2 or A2B kidneys in 25% of US transplant centers (128). Transplant centers are required to have local policies addressing acceptable anti-A titers in these candidates (Table 9). Gilbert et al. and Azzi et al. have reviewed ABO issues in A2-incompatible kidney transplants (129,130). Azzi et al. summarized 13 prior studies of A2-incompatible deceased- or living-donor kidneys, finding that 8 studies used anti-A1 titers and the rest anti-A2 titers (see ABO antibody titers section below) (130). Most follow IgG titers although some centers also report IgM levels. Azzi et al. successfully used anti-A2 IgG titers <16 as their acceptable level without plasma exchange. Outcomes in A2-incompatible kidney transplants have been similar to standard ABO-compatible grafts, and some have come to think of them as ABO-compatible by comparison with fully incompatible transplants (131).
Table 9
| Organ | Who | When | Titer limit |
|---|---|---|---|
| Kidney | B candidates for Asub or AsubB organs | Confirm eligible every 90 d | Program written policy for titer limit |
| Kidney paired donation | B candidates for Asub or AsubB organs | At listing | IgG <8 |
| O candidates for Asub organ | |||
| Pediatric heart: at listing | <1 yr old, status 1A or 1B | In past 30 d | None specified |
| 1 yr to <2 yr old, status 1A or 1B | In past 30 d | ≤16 and no recent titer reduction treatments | |
| If multiple titers/sample, report highest | |||
| Follow-up reports | Every 30 d | ||
| ≤24 hr pre–transplant | |||
| Graft loss if <1 yr | |||
| Last before death if <1 yr | |||
| Pediatric lung | All same as hearts, status priority 1 |
Organ Procurement and Transplantation Network (OPTN) Policies (44). Asub, A subgroup.
A2-incompatible liver transplants are also performed in selected patients. They comprised 1% of deceased-donor adult liver transplants in the US in 2013–2015, or about 60 per year (93).
Fully ABO-i kidney transplantation was reviewed by Hourmant et al. (132). Most reports have sought a preoperative IgG anti-A1 titer of <8, but some have used <16 or <32. One program successfully used IgM titers <4 regardless of IgG (133). A meta-analysis of 26 studies worldwide found that overall 1-year graft survival was 96% compared to 98% (P<0.001) in ABO-compatible transplants, and the rates of antibody mediated rejection were 10% vs. 2% (134). In the US, 1.3% of all living-donor adult renal transplants in 2000–2015 (930 cases, or about 60/year) were fully ABO-i (131). The absolute 1-year graft loss rate was not given but the adjusted hazard ratio was 2.34, similar to the literature meta-analysis of 4% vs. 2%. The 1-year prevalence of acute rejection episodes was 19% vs. 10%. Successful ABO-i kidney transplants undergo an incompletely understood process called accommodation in which graft function is maintained despite continued ABO antibody and C4d complement deposition. Mechanisms include downregulation of ABO plasma antibody and kidney ABO antigen levels and upregulation of renal complement regulatory molecules (135). Overall, good although not quite equivalent outcomes are achieved with ABO-i kidney transplants, and they expand organ availability for some patients such as those with broad HLA alloimmunization.
Infants do not produce RBC antibodies until at least 4 months of age and can become tolerant to antigens to which they are exposed at a young age. Because of the scarcity of neonatal and infant heart donors, fully ABO-i heart transplants for infants began in the 1990s and have become routine in some pediatric heart transplant programs. Kozik et al. examined US OPTN records from 2007–2018 (136). By the end of the period, 72% of heart transplant candidates under 2 years old were listed for ABO-i hearts and 25% of transplants were ABO-i. ABO-i heart recipients had survivals and 1-year rejection-episode rates equivalent to ABO-compatible recipients. Equivalent propensity-score-matched survivals were also seen in a large international registry of transplants from 1999 to 2018 (137). Infants receiving ABO-i hearts have long-term discrepancies in their ABO typings because of near-absence of ABO antibodies against the heart, and in particular some are missing antibodies to type 2 ABO glycans expressed in cardiac tissue (138).
OPTN policies for status 1A or 1B ABO-i pediatric heart transplant candidates are summarized in Table 9. No titer limit is specified for patients <1 year old. For patients between 1 and 2 years old, the anti-ABO titer threshold is <16 for listing. The titer method and whether IgG or IgM are not specified. If multiple titers are done on the same specimen, the highest titer must be reported. Dean et al. surveyed 21 US and Canadian transfusion services on their testing and transfusion practices in 2018 (139). Seventy-one percent performed both IgM and IgG titers. Half of the programs used cutoff titers other than 16 for antibody reduction therapy for high titers. Respondents were asked about whether they mitigated ABO antibody content of transfusions. About 50% gave washed or volume-reduced RBCs preoperatively or postoperatively, and 70% intraoperatively. Eighty percent to 90% gave plasma-rich products as group AB or for platelets, volume-reduced.
OPTN policies also permit priority 1 listing for ABO-i infant lung transplants, using the same criteria as for hearts. These are very uncommonly done. Costello et al. recently reviewed the limited available information (140).
Transfusion services supporting A2- and A1-incompatible transplants should have protocols in place to avoid giving plasma-rich blood components containing anti-A/B against the organ. Transplant services should notify the transfusion service when a patient is listed for ABO-i transplant so that ABO-appropriate plasma and platelets are given. Platelets can be washed or volume-reduced (2 hours processing time) for non-urgent needs if necessary. The small amount of plasma in additive-solution RBCs may not be significant except possibly in infants.
ABO antibody titers
ABO antibody titration in ABO-i organ transplant candidates and recipients is an important element of patient care. ABO antibody hemagglutination was the first clinical immunohematology test in the early 1900s and is one of the oldest laboratory tests still routinely performed. However, serial plasma dilutions, hemagglutinations and interpretations are all technique- and method-dependent. In manual tube titration, endpoints plus or minus one tube are generally accepted in blood banking as equivalent and within the limits of feasible precision. Exact titer thresholds such as those in the OPTN policies (Table 9) do not reflect this reality.
Group O persons usually have much higher IgG than IgM ABO titers, whereas group A and B persons have equal or higher IgM titers (141). As discussed in the transplant section, both IgG and IgM titers are often done in ABO-i transplant patients. Although IgG levels are most often monitored clinically, IgM antibodies more readily fix complement. Some laboratories titer IgG after IgM inactivation with dithiothreitol (142), but most do not (141).
The reproducibility of ABO titers across different laboratories is notoriously inexact. Proficiency testing (PT) programs receive a broad range of results for the same plasma. A US expert group studied this issue in 2008 and suggested a uniform method for reading endpoints (tube weak + antiglobulin phase) based on data from a referee panel (143). However, when this was applied for several years among >500 laboratories in a large PT program, agreement for the uniform method was no better than for others (144). Japanese and Korean laboratories went through analogous processes with more success, improving consensus on external quality assessments with standardized tube methods (142,145). Recently an Australasian pathology quality assurance program rediscovered widely variant titer results when external samples were tested across 24 laboratories with many different methods; e.g., anti-A1 titers on the same plasma ranged from 8 to 1,024 (146). In the United Kingdom, facilities whose laboratories reported higher titers on external-assessment specimens performed more plasma exchange procedures for ABO-i kidney transplants (147).
To seek more objective readouts and reduce hands-on time compared to tube hemagglutination, other methods have been examined. Johns Hopkins Hospital in Maryland was an early proponent of manual IgG gel titers (148). More recently they reported that automated dilution and hemagglutination on the solid-phase platform gave results generally equivalent to manual dilution and manual gel; group A and B samples were slightly higher in gel (141). Adkins et al. found that IgM anti-A and anti-B automated gel titers were comparable to tube direct agglutination and were equivalent across instruments and between two laboratories (149). Shim et al. compared manual tube, manual gel and automated erythrocyte-magnetized technology (EMT) titers (150) (EMT pulls reagent RBCs coated with iron particles to the bottom of microwells by magnetic force instead of centrifugation before dispersal or hemagglutination is assessed.). All 3 methods were comparable for IgM but IgG patterns varied by blood type and method. Responding to growing interest in automated-platform antibody titers, the CAP introduced proficiency testing in 2020. Flow cytometry has been investigated for detecting binding of titered antibodies to RBCs (151,152) and for assessing ABO antibody levels after ABO immunoadsorption (153).
But are RBCs actually the best target to assess anti-organ ABO antibodies? A and B antigens are synthesized on four main H-precursor carbohydrate structures whose distributions vary among organs. Table 10 compares A1 and A2 RBCs and organs with regard to ABH chain types. In the liver, the Type 1 ABH content of hepatic bile ducts is determined by secretor status. Type 2 structures are the major class on RBCs and in hearts. Most ABO antigens in kidneys are type 4, synthesized onto P antigens. RBCs have little type 4 antigen, and A2 RBCs, which have been advocated for titers to monitor A2-incompatible kidneys, have none.
Table 10
| Structure | Type 1—secretors | Type 2 | Type 3 | Type 4 | References |
|---|---|---|---|---|---|
| Locations | Endoderm; Secretions | Ectoderm; Endoderm; Secretions | Mucin; Glycolipids | Glycolipids | (154) |
| H precursors | H (Led) on Lec | H (CD173) | H on T | Globo-H on P | (154) |
| RBC A1 | From plasma | Major | Minor-glycolipids | Minor | (154,155) |
| A2 | None* | Reduced | Weak or none | None | |
| B | From plasma | Major | None | None | |
| Kidney A1 | Trace (whole kidney) | Minor: distal tubules; collecting ducts | Minor (whole kidney) | Major: distal tubules; collecting ducts | (154,156-158) |
| A2 | Reduced | ||||
| B | Trace | ||||
| Heart A1 & B | None | Positive | None | None | (155) |
| A2 | Reduced | ||||
| A2B | No A detected | ||||
| Liver A1 & B | Bile ducts, arteries | Some | Some | (157,158) | |
| A2 | Reduced |
*, Jeyakanthan et al. examined stored reagent RBCs (155). RBC, red blood cell.
The potential clinical significance of ABH structures is suggested by the work of Jeyakanthan et al., who assessed antibodies in pediatric heart transplant patients using glycan microarrays (155). As noted earlier, children with ABO-i hearts have reduced levels of anti-A or-B against their organs. Jeyakanthan et al. found that group O patients who received group A hearts are specifically missing IgM and IgG antibody to type 2 antigens borne by their hearts, but still have antibodies to types 1, 3 and 4.
Another emerging tool is the ability to introduce ABH-chain-specific antigens into RBCs. Carbohydrate structures of interest have been linked by spacers to glycolipids. When these constructs are mixed with RBCs, the RBC membranes take up the molecules and the RBCs then express the added antigens. The manufacturer, Kode Biotech (Auckland, NZ), terms such RBCs kodecytes. Type-2-augmented RBCs were evaluated for titrating ABO antibodies in candidates for ABO-i renal transplants (159).
Lindberg et al. adsorbed plasma ex vivo with types 1, 2, 3 or 4 group A and B tetrasaccharides on Sepharose beads (160). Partial type-specific removal was seen for IgG, but not for IgM.
ABO-i kidney transplants are nearly as successful as ABO-compatible transplants. However, graft survival is slightly lower and patients have more infections under extra humoral immunosuppression, and more bleeding complications after preoperative plasma removal procedures (132). If ABO antibodies to organ-predominant ABO antigen structures—type 1 in livers, type 2 in hearts, type 4 in kidneys—could be assayed using targets like glycan arrays or modified RBCs, and reduced in vivo by more focused structure-specific immunoadsorption, perhaps outcomes could be improved with less adverse events and the ABO barrier could be overcome for more patients.
Therapeutic apheresis
Therapeutic apheresis (TA) is employed in organ transplantation to remove HLA or ABO antibodies before or after transplant or to treat graft rejection. At active transplant centers, these treatments constitute a significant portion of the apheresis program’s activities. Table 11 shows the current indications for apheresis in organ transplantation in guidelines of the American Society for Apheresis (ASFA) (161). Therapeutic plasma exchange (TPE) is mostly recommended for HLA donor-specific antibody (DSA) removal during pre- or post-transplant desensitization or to help treat antibody-mediated rejection (AMR). Immunoadsorption (IA) removes antibodies by running plasma through devices which bind immunoglobulin (e.g., Staphylococcus protein A) or ABO antibodies (ABO glycans). (IA devices are not available in the US except in research protocols.) Extracorporeal photopheresis (ECP) is employed in liver, heart and lung transplants to treat or prevent rejection. TA is usually performed in conjunction with other measures to suppress humoral or cellular immunity as indicated.
Table 11
| Organ | Indication | Procedures | Category | Grade |
|---|---|---|---|---|
| Kidney ABO-c | Desensitization LD | TPE/IA | I | 1B |
| Antibody mediated rejection | TPE/IA | I | 1B | |
| Desensitization DD | TPE/IA | III | 2C | |
| Kidney ABO-i | Desensitization LD | TPE/IA | I | 1B |
| Antibody mediated rejection | TPE/IA | II | 1B | |
| Liver ABO-i | Desensitization LD | TPE | I | 1C |
| Desensitization DD | TPE | III | 2C | |
| Desensitization | ECP | III | 2C | |
| Liver | Acute rejection | ECP | III | 2B |
| Immune suppression withdrawal | ECP | III | 2B | |
| Antibody mediated rejection | TPE | III | 2C | |
| Heart | Rejection prophylaxis | ECP | II | 2A |
| Cellular/recurrent rejection | ECP | II | 1B | |
| Desensitization | TPE | II | 1C | |
| Antibody mediated rejection | TPE | III | 2C | |
| Lung | Bronchiolitis obliterans | ECP | II | 1C |
| Desensitization | TPE | III | 2C | |
| Antibody mediated rejection | TPE | III | 2C |
From 2019 ASFA guidelines (161). Within each organ group, indications are listed from higher to lower categories and evidence grades. Categories: I, first-line therapy; II, second-line therapy; III, optimum role not established. Grade of evidence: recommendation strong [1] or weak [2]. Quality of evidence high (A), moderate (B) or low (C). ABO-c, ABO-compatible; ABO-I, ABO-incompatible; DD, deceased donor; ECP, extracorporeal photopheresis; IA, immunoadsorption; LD, living donor; TPE, therapeutic plasma exchange.
Abbes et al. reviewed HLA antibody testing methods in the context of organ transplants and TA (162). Eighteen to 30% of candidates are HLA-sensitized and around 15% develop new antibodies post-transplant. Although cell-based cytotoxicity testing is still sometimes done, especially to assess complement fixation, most antibody testing utilizes solid-phase Class I and II antigens. Candidates are screened for HLA antibodies and evaluated for DSA when a transplant is considered. HLA laboratories have individualized methods for evaluating antibody levels with fluorescence intensities and titers.
Experts from the AABB Apheresis Committee provided a practical overview of TA practices in transplantation (163). For desensitization, pre-treatment ABO or HLA antibody titers help determine the feasibility and number of TA procedures needed. TPE is often performed every other day to allow for equilibration of extravascular IgG into plasma for the next procedure, although in acute AMR, some centers start with several daily procedures. Replacement fluid is usually albumin unless plasma is needed for hemostasis perioperatively or during bleeding.
In ECP, peripheral blood mononuclear cells (MNCs) are separated, exposed to 8-methoxypsoralen (8-MOP) either by administration to the patient or ex vivo, and irradiated with ultraviolet A (UVA) light to induce nucleic acid crosslinking by 8-MOP. ECP is done either by dedicated photopheresis instruments with in-line irradiation or by treating collected MNCs ex vivo and reinfusing separately. The treated MNCs then undergo apoptosis over 1 to 2 days.
In the US photopheresis devices are FDA-approved for treating cutaneous T-cell lymphoma. The mechanisms of immunomodulation for treatment of heart, liver or lung rejection are uncertain. Phagocytosis of apoptotic MNCs may induce a shift from inflammatory to anti-inflammatory cytokines and increased T-regulatory cells (164). Some UVA-irradiated MNCs may survive and become tolerogenic dendritic cells (165). ECP is often scheduled in a cycle of two treatments on consecutive days. Treatment courses are variable and response-dependent. ASFA guidelines give examples in cardiac rejection of cycles every 2–8 weeks for several months, and in lung-transplant bronchiolitis obliterans syndrome of 12 gradually spaced-out cycles over 6 months.
ECP is not included in the 2019 ASFA guidelines for renal transplants. In 2019 Tamain et al. reported retrospective experience with 33 cases of renal rejection treated with ECP because standard therapies failed or were contraindicated (Tamain). Patients initially received 1–2 treatments/week, tapered to monthly treatments as long as their graft survived. One-year graft survival was 61%. Of note were 6 patients with AMR in whom standard steroids, TPE and intravenous immune globulin (IVIG) or rituximab either failed (n=1) or became contraindicated by infection (n=5), and 1 patient who was switched from TPE to IVIG due to septicemia. All 7 grafts survived.
Conclusions
Some key conclusions can be drawn from this overview. The transfusion needs of liver, heart and lung transplant patients are usually manageable but sometimes challenging. As with other major operations, high transfusions are associated with adverse outcomes, and proactive patient blood management can reduce transfusions. ABO-i organ transplants are a very active area of development, especially for A2- and A1-incompatible kidneys. Anti-A/B titers are a key laboratory contribution, but more method standardization is needed. Because the predominant precursor ABH structures vary by organ—type 1 in livers, type 2 in hearts and type 4 in kidneys—future research is in order to determine whether structure-specific antibody levels and fine-specificity adsorption techniques can improve outcomes. Therapeutic apheresis plays a major role in preventing and treating organ rejection, but better understanding of how ECP works and how to best employ it could also be beneficial.
In the introduction we cited GODT’s surveillance data that worldwide organ transplants had risen by 52% over the most recent 11 years of available data. Soberingly, we can conclude with their estimate that this still meets no more than 10% of the current global transplant needs. As the field of organ transplantation works to expands its reach and improve its successes, transfusion medicine will continue to have a vital role in its progress.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Paul D. Mintz) for the series “Transfusion Therapy: Principles and Practices” published in Annals of Blood. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://aob.amegroups.com/article/view/10.21037/aob-21-72/coif). The series “Transfusion Therapy: Principles and Practices” was commissioned by the editorial office without any funding or sponsorship. GR is the chair of the College of American Pathologists Transfusion, Apheresis and Cellular Therapy Committee. This committee oversees CAP proficiency testing programs for ABO subgroups and ABO antibody titers which are used in organ transplants and are mentioned in this article. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Organ Donation and Transplantation Activities 2008 report. Global Observatory on Donation and Transplantation, 2008. Accessed online: http://www.transplant-observatory.org
- Organ Donation and Transplantation Activities 2019 report. Global Observatory on Donation and Transplantation, April 2021. Accessed online: http://www.transplant-observatory.org
- Organ Procurement and Transplantation Network (OPTN) Data. Richmond, VA: OPTN and United Network for Organ Sharing, September 1, 2021. Accessed online: https://optn.transplant.hrsa.gov/data
- Butler P, Israel L, Nusbacher J, et al. Blood transfusion in liver transplantation. Transfusion 1985;25:120-3. [Crossref] [PubMed]
- Nedelcu E, Wright MF, Karp S, et al. Quality improvement in transfusion practice of orthotopic liver transplantation reduces blood utilization, length of hospital stay, and cost. Am J Clin Pathol 2019;151:395-402. [Crossref] [PubMed]
- Sakai T, Matsusaki T, Dai F, et al. Pulmonary thromboembolism during adult liver transplantation: incidence, clinical presentation, outcome, risk factors, and diagnostic predictors. Br J Anaesth 2012;108:469-77. [Crossref] [PubMed]
- Abuelkasem E, Mazzeffi MA, Lu SY, et al. Ex vivo evaluation of 4 different viscoelastic assays for detecting moderate to severe coagulopathy during liver transplantation. Liver Transpl 2016;22:468-75. [Crossref] [PubMed]
- McCluskey SA, Karkouti K, Wijeysundera DN, et al. Derivation of a risk index for the prediction of massive blood transfusion in liver transplantation. Liver Transpl 2006;12:1584-93. [Crossref] [PubMed]
- Badenoch A, Sharma A, Gower S, et al. The effectiveness and safety of tranexamic acid in orthotopic liver transplantation clinical practice: a propensity score matched cohort study. Transplantation 2017;101:1658-65. [Crossref] [PubMed]
- Metcalf RA, Pagano MB, Hess JR, et al. A data-driven patient blood management strategy in liver transplantation. Vox Sang 2018;113:421-9. [Crossref] [PubMed]
- Pustavoitau A, Rizkalla NA, Perlstein B, et al. Validation of predictive models identifying patients at risk for massive transfusion during liver transplantation and their potential impact on blood bank resource utilization. Transfusion 2020;60:2565-80. [Crossref] [PubMed]
- Uzuni A, El-Bashir J, Galusca D, et al. Transfusion requirements and alloimmunization to red blood cell antigens in orthotopic liver transplantation. Vox Sang 2022;117:408-14. [Crossref] [PubMed]
- Shaylor R, Desmond F, Lee DK, et al. The impact of intraoperative donor blood on packed red blood cell transfusion during deceased donor liver transplantation: a retrospective cohort study. Transplantation 2021;105:1556-63. [Crossref] [PubMed]
- Kirchner C, Dirkmann D, Treckmann JW, et al. Coagulation management with factor concentrates in liver transplantation: a single-center experience. Transfusion 2014;54:2760-8. [Crossref] [PubMed]
- Massicotte L, Denault AY, Beaulieu D, et al. Transfusion rate for 500 consecutive liver transplantations: experience of one liver transplantation center. Transplantation 2012;93:1276-81. [Crossref] [PubMed]
- Jabbour N, Gagandeep S, Mateo R, et al. Transfusion free surgery: single institution experience of 27 consecutive liver transplants in Jehovah's Witnesses. J Am Coll Surg 2005;201:412-7. [Crossref] [PubMed]
- Costanzo D, Bindi M, Ghinolfi D, et al. Liver transplantation in Jehovah's witnesses: 13 consecutive cases at a single institution. BMC Anesthesiol 2020;20:31. [Crossref] [PubMed]
- Frasco PE, Poterack KA, Hentz JG, et al. A comparison of transfusion requirements between living donation and cadaveric donation liver transplantation: relationship to model of end-stage liver disease score and baseline coagulation status. Anesth Analg 2005;101:30-7. table of contents. [Crossref] [PubMed]
- Li C, Wen TF, Yan LN, et al. Factors associated with early mortality after living-donor liver transplant. Exp Clin Transplant 2015;13:62-7. [PubMed]
- Nafea MA, Alsebaey A, Abd El Aal Sultan A, et al. Predictors of early recipient mortality after living donor liver transplantation in a tertiary care center in Egypt. Ann Saudi Med 2019;39:337-44. [Crossref] [PubMed]
- Nacoti M, Cazzaniga S, Lorusso F, et al. The impact of perioperative transfusion of blood products on survival after pediatric liver transplantation. Pediatr Transplant 2012;16:357-66. [Crossref] [PubMed]
- Fanna M, Baptiste A, Capito C, et al. Preoperative risk factors for intra-operative bleeding in pediatric liver transplantation. Pediatr Transplant 2016;20:1065-71. [Crossref] [PubMed]
- Tran LT, Mazariegos GV, Damian D, et al. Red blood cell transfusion in pediatric orthotopic liver transplantation: what a difference a few decades make. Anesth Analg 2019;129:1087-92. [Crossref] [PubMed]
- Kloesel B, Kovatsis PG, Faraoni D, et al. Incidence and predictors of massive bleeding in children undergoing liver transplantation: A single-center retrospective analysis. Paediatr Anaesth 2017;27:718-25. [Crossref] [PubMed]
- Villarreal JA, Yoeli D, Ackah RL, et al. Intraoperative blood loss and transfusion during primary pediatric liver transplantation: A single-center experience. Pediatr Transplant 2019;23:e13449. [Crossref] [PubMed]
- Rössler F, Sapisochin G, Song G, et al. Defining benchmarks for major liver surgery: a multicenter analysis of 5202 living liver donors. Ann Surg 2016;264:492-500. [Crossref] [PubMed]
- Ramsey G, Schmidt PJ. Transfusion medicine in Chicago, before and after the "blood bank". Transfus Med Rev 2009;23:310-21. [Crossref] [PubMed]
- Avtaar Singh SS, Banner NR, Rushton S, et al. ISHLT primary graft dysfunction incidence, risk factors, and outcome: a UK national study. Transplantation 2019;103:336-43. [Crossref] [PubMed]
- Subramaniam K, Kumar A, Hernandez S, et al. Effect of blood product transfusion on perioperative outcomes after heart transplantation. J Cardiothorac Vasc Anesth 2021;35:1067-72. [Crossref] [PubMed]
- Pratt Cleary J, Hodge L, Palmer B, et al. 4-Factor Prothrombin Complex Concentrate (PCC4, Kcentra®) protocol reduces blood requirements for heart transplantation: a novel protocol. Ann Transplant 2016;21:531-7. [Crossref] [PubMed]
- Enter DH, Zaki AL, Marsh M, et al. Prothrombin complex concentrate reduces blood product utilization in heart transplantation. Pharmacotherapy 2017;37:1215-20. [Crossref] [PubMed]
- Wanek MR, Hodges K, Persaud RA, et al. Prothrombin complex concentrates for warfarin reversal before heart transplantation. Ann Thorac Surg 2019;107:1409-15. [Crossref] [PubMed]
- Sun GH, Patel V, Moreno-Duarte I, et al. Intraoperative administration of 4-factor prothrombin complex concentrate reduces blood requirements in cardiac transplantation. J Cardiothorac Vasc Anesth 2018;32:161-7. [Crossref] [PubMed]
- Ong LP, Thompson E, Sachdeva A, et al. Allogeneic blood transfusion in bilateral lung transplantation: impact on early function and mortality. Eur J Cardiothorac Surg 2016;49:668-74; discussion 674. [Crossref] [PubMed]
- Ong LP, Sachdeva A, Ramesh BC, et al. Lung transplant with cardiopulmonary bypass: impact of blood transfusion on rejection, function, and late mortality. Ann Thorac Surg 2016;101:512-9. [Crossref] [PubMed]
- Smith I, Pearse BL, Faulke DJ, et al. Targeted bleeding management reduces the requirements for blood component therapy in lung transplant recipients. J Cardiothorac Vasc Anesth 2017;31:426-33. [Crossref] [PubMed]
- Durila M, Vajter J, Garaj M, et al. Rotational thromboelastometry reduces blood loss and blood product usage after lung transplantation. J Heart Lung Transplant 2021;40:631-41. [Crossref] [PubMed]
- Bharat A, Machuca TN, Querrey M, et al. Early outcomes after lung transplantation for severe COVID-19: a series of the first consecutive cases from four countries. Lancet Respir Med 2021;9:487-97. [Crossref] [PubMed]
- Huddleston SJ, Jackson S, Kane K, et al. Separate effect of perioperative recombinant human factor VIIa administration and packed red blood cell transfusions on midterm survival in lung transplantation recipients. J Cardiothorac Vasc Anesth 2020;34:3013-20. [Crossref] [PubMed]
- Seay T, Guinn N, Maisonave Y, et al. The association of increased FFP:RBC transfusion ratio to primary graft dysfunction in bleeding lung transplantation patients. J Cardiothorac Vasc Anesth 2020;34:3024-32. [Crossref] [PubMed]
- Borders CF, Suzuki Y, Lasky J, et al. Massive donor transfusion potentially increases recipient mortality after lung transplantation. J Thorac Cardiovasc Surg 2017;153:1197-1203.e2. [Crossref] [PubMed]
- Lin SS. TRALI by proxy. J Thorac Cardiovasc Surg 2017;153:1204-5. [Crossref] [PubMed]
- Vossoughi S, Gorlin J, Kessler DA, et al. Ten years of TRALI mitigation: measuring our progress. Transfusion 2019;59:2567-74. [Crossref] [PubMed]
- Organ Procurement and Transplantation Network (OPTN) Policies. Richmond, VA: OPTN and United Network for Organ Sharing, September 1, 2021. Accessed online: https://optn.transplant.hrsa.gov/governance/policies/
- Surgical blood order schedule. Department of Anesthesiology, Johns Hopkins Hospital, Baltimore, MD, 2016. Accessed online: https://anesthesiology.hopkinsmedicine.org/wp-content/uploads/2016/10/Blood-Order-Schedule-v4.pdf
- Callaghan CJ, Phillips BL, Foukaneli T, et al. The use of third-party packed red blood cells during ex situ normothermic machine perfusion of organs for transplantation: Underappreciated complexities? Am J Transplant 2021;21:1376-81. [Crossref] [PubMed]
- Elliot J, Narayan S, Poles D, et al. Missed irradiation of cellular blood components for vulnerable patients: Insights from 10years of SHOT data. Transfusion 2021;61:385-92. [Crossref] [PubMed]
- O'Brien KL, Pereira SE, Wagner J, et al. Transfusion-associated graft-versus-host disease in a liver transplant recipient: an unusual presentation and review of the literature. Transfusion 2013;53:174-80. [Crossref] [PubMed]
- Pritchard AE, Shaz BH. Survey of Irradiation Practice for the Prevention of Transfusion-Associated Graft-versus-Host Disease. Arch Pathol Lab Med 2016;140:1092-7. [Crossref] [PubMed]
- Triulzi DJ. Specialized transfusion support for solid organ transplantation. Curr Opin Hematol 2002;9:527-32. [Crossref] [PubMed]
- Hod EA, Francis RO. Noninfectious complications of blood transfusion. In: Cohn CS, Delaney M, Johnson ST, et al. Technical manual. 20th ed. Bethesda, MD: AABB, 2020:627-57.
- CAMPATH (alemtuzumab) injection, for intravenous use. Prescribing information. Cambridge, MA: Genzyme Corporation, October 2020. Accessed online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/103948s5171lbl.pdf
- Lemtrada (alemtuzumab) injection, for intravenous use. Prescribing information. Cambridge, MA: Genzyme Corporation, April 2021. Accessed online: https://products.sanofi.us/lemtrada/lemtrada.html
- Kopolovic I, Ostro J, Tsubota H, et al. A systematic review of transfusion-associated graft-versus-host disease. Blood 2015;126:406-14. [Crossref] [PubMed]
- Hui YM, Regan F, Willecombe M, et al. Use of non-irradiated blood components in Campath (alemtuzumab)-treated renal transplant patients. Transfus Med 2016;26:138-46. [Crossref] [PubMed]
- Foukaneli T, Kerr P, Bolton-Maggs PHB, et al. Guidelines on the use of irradiated blood components. Br J Haematol 2020;191:704-24. [Crossref] [PubMed]
- Ramsey G, Cornell FW, Hahn LF, et al. Red cell antibody problems in 1000 liver transplants. Transfusion 1989;29:396-400. [Crossref] [PubMed]
- Motschman TL, Taswell HF, Brecher ME, et al. Blood bank support of a liver transplantation program. Mayo Clin Proc 1989;64:103-11. [Crossref] [PubMed]
- Shariatmadar S, Pyrsopoulos NT, Vincek V, et al. Alloimmunization to red cell antigens in liver and multivisceral transplant patients. Transplantation 2007;84:527-31. [Crossref] [PubMed]
- Au WY, Liu CL, Lo CM, et al. Red blood cell alloantibodies and liver transplantation in Chinese patients. Transplantation 2003;76:324-6. [Crossref] [PubMed]
- Luzo AC, Pereira FB, de Oliveira RC, et al. Red blood cell antigen alloimmunization in liver transplant recipients. Transplant Proc 2010;42:494-5. [Crossref] [PubMed]
- Boyd SD, Stenard F, Lee DK, et al. Alloimmunization to red blood cell antigens affects clinical outcomes in liver transplant patients. Liver Transpl 2007;13:1654-61. [Crossref] [PubMed]
- Mushkbar M, Watkins E, Doughty H. A UK single-centre survey of red cell antibodies in adult patients undergoing liver transplantation. Vox Sang 2013;105:341-5. [Crossref] [PubMed]
- Solves P, Carpio N, Moscardo F, et al. Transfusion management and immunohematologic complications in liver transplantation: experience of a single institution. Transfus Med Hemother 2015;42:8-14. [Crossref] [PubMed]
- Ramsey G, Cornell FW, Hahn LF, et al. Incompatible blood transfusions in liver transplant patients with significant red cell alloantibodies. Transplant Proc 1989;21:3531. [PubMed]
- Piccoli PL, Franchini M, Gandini G, et al. Transfusional management of a patient with anti-PP1Pk alloantibody undergoing liver transplantation. Transplantation 2006;81:1604-5. [Crossref] [PubMed]
- Kurata N, Onishi Y, Kamei H, et al. Successful Blood Transfusion Management of a Living Donor Liver Transplant Recipient in the Presence of Anti-Jra: A Case Report. Transplant Proc 2017;49:1604-7. [Crossref] [PubMed]
- Thonier V, Cohen-Bacrie S, Loussert I, et al. Management of the blood supply for a Jk(a-b-) patient with an anti-Jk3 in preparation for an urgent heart transplant: An illustrative example of a successful international cooperation. Transfus Clin Biol 2019;26:48-55. [Crossref] [PubMed]
- Irani MS, Karafin MS, Ernster L. Red cell exchange to mitigate a delayed hemolytic transfusion reaction in a patient transfused with incompatible red blood cells. J Clin Apher 2017;32:59-61. [Crossref] [PubMed]
- Yazer MH, Triulzi DJ, Sperry JL, et al. Rate of RhD-alloimmunization after the transfusion ofmultiple RhD-positive primary red blood cell-containing products. Transfusion 2021;61:S150-8. [Crossref] [PubMed]
- Ramsey G, Hahn LF, Cornell FW, et al. Low rate of Rhesus immunization from Rh-incompatible blood transfusions during liver and heart transplant surgery. Transplantation 1989;47:993-5. [Crossref] [PubMed]
- Casanueva M, Valdes MD, Ribera MC. Lack of alloimmunization to D antigen in D-negative immunosuppressed liver transplant recipients. Transfusion 1994;34:570-2. [Crossref] [PubMed]
- Yuan S, Davis R, Lu Q, et al. Low risk of alloimmunization to the D antigen in D- orthotopic liver transplant recipients receiving D+ RBCs perioperatively. Transfusion 2008;48:2653-5. [Crossref] [PubMed]
- Stevens J, Callender CO, Jilly PN. Emergence of red blood cell agglutinins following renal transplantation in a patient with systemic lupus erythematosus. Transplantation 1981;32:398-400. [Crossref] [PubMed]
- Ramsey G, Nusbacher J, Starzl TE, et al. Isohemagglutinins of graft origin after ABO-unmatched liver transplantation. N Engl J Med 1984;311:1167-70. [Crossref] [PubMed]
- Ramsey G. Red cell antibodies arising from solid organ transplants. Transfusion 1991;31:76-86. [Crossref] [PubMed]
- Ramsey G, Israel L, Lindsay GD, et al. Anti-Rho(D) in two Rh-positive patients receiving kidney grafts from an Rh-immunized donor. Transplantation 1986;41:67-9. [Crossref] [PubMed]
- Nadarajah L, Ashman N, Thuraisingham R, et al. Literature review of passenger lymphocyte syndrome following renal transplantation and two case reports. Am J Transplant 2013;13:1594-600. [Crossref] [PubMed]
- Romero S, Solves P, Lancharro A, et al. Passenger lymphocyte syndrome in liver transplant recipients: a description of 12 cases. Blood Transfus 2015;13:423-8. [PubMed]
- Moosavi MM, Duncan A, Stowell SR, et al. Passenger lymphocyte syndrome; a review of the diagnosis, treatment, and proposed detection protocol. Transfus Med Rev 2020;34:178-87. [Crossref] [PubMed]
- Triulzi DJ, Shirey RS, Ness PM, et al. Immunohematologic complications of ABO-unmatched liver transplants. Transfusion 1992;32:829-33. [Crossref] [PubMed]
- Kunimasa J, Yurugi K, Ito K, et al. Hemolytic reaction due to graft-versus-host (GVH) antibody production after liver transplantation from living donors: report of two cases. Surg Today 1998;28:857-61. [Crossref] [PubMed]
- ElAnsary M, Hanna MO, Saadi G, et al. Passenger lymphocyte syndrome in ABO and Rhesus D minor mismatched liver and kidney transplantation: A prospective analysis. Hum Immunol 2015;76:447-52. [Crossref] [PubMed]
- de Bruijn S, Philipse E, Couttenye MM, et al. Passenger lymphocyte syndrome (PLS): a single-center retrospective analysis of minor ABO-incompatible liver transplants. J Clin Transl Hepatol 2017;5:9-15. [Crossref] [PubMed]
- Woolfson JP, Vandriel SM, Stephens D, et al. Passenger lymphocyte syndrome after pediatric liver transplantation. J Pediatr Gastroenterol Nutr 2019;69:95-101. [Crossref] [PubMed]
- Brunetta DM, de Barros Carlos LM, Da Silva VFP, et al. Prospective evaluation of immune haemolysis in liver transplantation. Vox Sang 2020;115:72-80. [Crossref] [PubMed]
- Povlsen JV, Rasmussen A, Hansen HE, et al. Acquired haemolytic anaemia due to isohaemagglutinins of donor origin following ABO-minor-incompatible kidney transplantation. Nephrol Dial Transplant 1990;5:148-51. [Crossref] [PubMed]
- Elhence P, Sharma RK, Chaudhary RK, et al. Acquired hemolytic anemia after minor ABO incompatible renal transplantation. J Nephrol 1998;11:40-3. [PubMed]
- Bakr MA, Abbas TM, Mustafa A, et al. Hemolytic anemia after ABO nonidentical living donor kidney transplantation. Clin Exp Nephrol 2009;13:161-5. [Crossref] [PubMed]
- Achkar R, Chiba AK, Zampieri-Filho JP, et al. Hemolytic anemia after kidney transplantation: a prospective analysis. Transfusion 2011;51:2495-9. [Crossref] [PubMed]
- Aujayeb A, Lordan J, Kilner M, et al. The passenger lymphocyte syndrome--experience from a cardiothoracic transplant unit. Transfus Med 2014;24:423-5. [Crossref] [PubMed]
- Thomas W, Foukaneli T, Cosgrove J, et al. Transplant-associated thrombotic microangiopathy and immune haematological complications following intestine-containing organ transplantation: experience from over 100 consecutive cases. Br J Haematol 2021;193:961-70. [Crossref] [PubMed]
- Ge J, Roberts JP, Lai JC. Race/ethnicity is associated with ABO-nonidentical liver transplantation in the United States. Clin Transplant 2017;31:e13011. [Crossref] [PubMed]
- Ainsworth CD, Crowther MA, Treleaven D, et al. Severe hemolytic anemia post-renal transplantation produced by donor anti-D passenger lymphocytes: case report and literature review. Transfus Med Rev 2009;23:155-9. [Crossref] [PubMed]
- Draper NL, Kallan JE. Passenger lymphocyte syndrome. In: Draper NL. editor. Chimerism: a clinical guide. Cham, Switzerland: Springer International, 2018:119-34.
- Turiño-Luque J, Zambudio-Carroll N, Muffak-Granero K, et al. Early detection of biliary complications and graft rejection in a non-RH identitical liver transplant recipient from a non-heart-beating donor: a case report. Transplant Proc 2012;44:2124-5. [Crossref] [PubMed]
- Gniadek TJ, McGonigle AM, Shirey RS, et al. A rare, potentially life-threatening presentation of passenger lymphocyte syndrome. Transfusion 2017;57:1262-6. [Crossref] [PubMed]
- Tsang HC, Samraj AN, Morse RJ, et al. Genetic testing to resolve the source of haemolytic antibody in solid organ transplantation. Blood Transfus 2019;17:307-11. [PubMed]
- Karanth P, Birchall J, Day S, et al. Immune hemolysis resulting from passenger lymphocyte syndrome derived anti-rh (D) reactivity after kidney transplantation: a case report and literature review. Transplantation 2014;97:e54-5. [Crossref] [PubMed]
- Cserti-Gazdewich CM, Waddell TK, Singer LG, et al. Passenger lymphocyte syndrome with or without immune hemolytic anemia in all Rh-positive recipients of lungs from rhesus alloimmunized donors: three new cases and a review of the literature. Transfus Med Rev 2009;23:134-45. [Crossref] [PubMed]
- Kim BK, Whitsett CF, Hillyer CD. Donor origin Rh antibodies as a cause of significant hemolysis following ABO-identical orthotopic liver transplantation. Immunohematology 1992;8:100-1. [Crossref] [PubMed]
- Seltsam A, Hell A, Heymann G, et al. Donor-derived alloantibodies and passenger lymphocyte syndrome in two of four patients who received different organs from the same donor. Transfusion 2001;41:365-70. [Crossref] [PubMed]
- Hareuveni M, Merchav H, Austerlitz N, et al. Donor anti-Jk(a) causing hemolysis in a liver transplant recipient. Transfusion 2002;42:363-7. [Crossref] [PubMed]
- Grosskreutz C, Gudzowaty O, Shi P, et al. Partial HLA matching and RH incompatibility resulting in graft versus host reaction and Evans syndrome after liver transplantation. Am J Hematol 2008;83:599-601. [Crossref] [PubMed]
- Shortt J, Westall GP, Roxby D, et al. A 'dangerous' group O donor: severe hemolysis in all recipients of organs from a donor with multiple red cell alloantibodies. Am J Transplant 2008;8:711-4. [Crossref] [PubMed]
- De Luna MMI, Behan KJ. ABO discrepancy and hemolyitc anemia post liver transplant due to passenger lymphocyte syndrome. Lab Med 2011;42:137-9. [Crossref]
- Koepsell SA, Landmark JD. Passenger lymphocyte syndrome: use of archived donor organ biopsy obtained at the time of transplantation for diagnosis. Am J Transplant 2013;13:2227. [Crossref] [PubMed]
- Schwartz D, Götzinger P. Immune-haemolytic anaemia (IHA) after solid organ transplantation due to rhesus antibodies of donor origin: report of 5 cases. Beitr Infusionsther 1992;30:367-9. [PubMed]
- Larrea L, de la Rubia J, Arriaga F, et al. Severe hemolytic anemia due to anti-E after renal transplantation. Transplantation 1997;64:550-1. [Crossref] [PubMed]
- Hurtarte-Sandoval AR, Navarro-Cabello MD, Álvarez-Rivas MA, et al. Passenger lymphocyte syndrome after simultaneous pancreas-kidney transplantation: a case report of an unusual cause of alloimmune hemolytic anemia. Transplant Proc 2015;47:2667-8. [Crossref] [PubMed]
- Makuria AT, Langeberg A, Fishbein TM, et al. Nonhemolytic passenger lymphocyte syndrome: donor-derived anti-M in an M+ recipient of a multiorgan transplant. Immunohematology 2009;25:20-3. [Crossref] [PubMed]
- Friend PJ, McCarthy LJ, Filo RS, et al. Transmission of idiopathic (autoimmune) thrombocytopenic purpura by liver transplantation. N Engl J Med 1990;323:807-11. [Crossref] [PubMed]
- Aranda Escaño E, Prieto Calvo M, Perfecto Valero A, et al. Transplantation-mediated alloimmune thrombocytopenia successfully treated by retransplantation. Lupus 2021;30:669-73. [PubMed]
- French W, Hopkins M, Poles A, et al. Passenger lymphocyte thrombocytopenia due to human platelet antigen 3a antibodies: case report and review of literature. Transfusion 2020;60:2185-8. [Crossref] [PubMed]
- Lindholm PF, Kwaan HC, Ramsey G, et al. Severe thrombocytopenia in a patient following liver transplantation caused by HPA-1a antibodies produced by the liver donor. Am J Hematol 2018;93:150-3. [Crossref] [PubMed]
- Hisatake GM, Chen TW, Renz JF, et al. Acquired hemophilia A after liver transplantation: a case report. Liver Transpl 2003;9:523-6. [Crossref] [PubMed]
- Maxfield SJ, Taylor CJ, Kosmoliaptsis V, et al. Transfer of hla-specific allosensitization from a highly sensitized deceased organ donor to the recipients of each kidney. Am J Transplant 2015;15:2501-6. [Crossref] [PubMed]
- Kummrow M, Hiho S, Hudson F, et al. Transfer of donor anti-HLA antibody expression to multiple transplant recipients: a potential variant of the passenger lymphocyte syndrome? Am J Transplant 2019;19:1577-81. [Crossref] [PubMed]
- Koshizuka T, Matsuda Y, Suzuki H, et al. Detection of engraftment of donor-derived antibody producing cells in a lung transplant recipient by anti-cytomegalovirus IgG avidity test. Transpl Immunol 2019;53:34-7. [Crossref] [PubMed]
- Smibert OC, Doyle JS, Pilcher D, et al. Unexplained persistent hepatitis C seropositivity (Hepc Ab+Ve) in the absence of viremia in lung transplant (Ltx) recipients from Hepc Ab+Ve/nucleic acid test negative (NAT-Ve) donors associated with excellent clinical outcomes and implications for future practice J Heart Lung Transplant 2018;37:S77. (abstract). [Crossref]
- Muller YD, Vionnet J, Beyeler F, et al. Management of allergy transfer upon solid organ transplantation. Am J Transplant 2020;20:834-43. [Crossref] [PubMed]
- Guidance for ABO subtyping organ donors for blood types A and AB. Richmond, VA: OPTN/UNOS, June 2018. Accessed online: https://optn.transplant.hrsa.gov/resources/guidance/
- Zhou Y, Wang Y, Ni H, et al. The potential significance of ABO genotyping for donor selection in kidney transplantation. Front Immunol 2020;11:608716. [Crossref] [PubMed]
- Ramsey G, Abecassis MI, Barnard C, et al. Preventing ABO blood group errors in organ transplantation, using blood transfusion as a model system Transfusion 2004;44:132A. (abstract).
- Olsson ML, Westman JS. ABO and other carbohydrate blood group systems. In: Cohn CS, Delaney M, Johnson ST, et al. Technical manual. 20th ed. Bethesda, MD: AABB, 2020:297-327.
- Mourant AE, Kopec AC, Domaniewska-Sobczak K. The distribution of the human blood groups and other polymorphisms. London: Oxford University Press, 1976.
- Rossmann SN, Ramsey G, Nash TA, et al. ABO subgroup proficiency-testing performance: implications for organ transplantation Transfusion 2021;61:121A. (abstract).
- Martins PN, Mustian MN, MacLennan PA, et al. Impact of the new kidney allocation system A2/A2B → B policy on access to transplantation among minority candidates. Am J Transplant 2018;18:1947-53. [Crossref] [PubMed]
- Gilbert AJ. Kidney transplantation across minor ABO incompatibility: the use of A2 to B transplants. Curr Opin Organ Transplant 2019;24:365-9. [Crossref] [PubMed]
- Azzi Y, Nair G, Loarte-Campos P, et al. A safe anti-A2 titer for a successful A2 incompatible kidney transplantation: a single-center experience and review of the literature. Transplant Direct 2021;7:e662. [Crossref] [PubMed]
- Mustian MN, Cannon RM, MacLennan PA, et al. Landscape of ABO-Incompatible live donor kidney transplantation in the US. J Am Coll Surg 2018;226:615-21. [Crossref] [PubMed]
- Hourmant M, Figueres L, Gicquel A, et al. New rules of ABO-compatibility in kidney transplantation. Transfus Clin Biol 2019;26:180-3. [Crossref] [PubMed]
- Kim H, Choe W, Shin S, et al. ABO-incompatible kidney transplantation can be successfully conducted by monitoring IgM isoagglutinin titers during desensitization. Transfusion 2020;60:598-606. [Crossref] [PubMed]
- de Weerd AE, Betjes MGH. ABO-incompatible kidney transplant outcomes: a meta-analysis. Clin J Am Soc Nephrol 2018;13:1234-43. [Crossref] [PubMed]
- Cen M, Wang R, Kong W, et al. ABO-incompatible living kidney transplantation. Clin Transplant 2020;34:e14050. [Crossref] [PubMed]
- Kozik D, Sparks J, Trivedi J, et al. ABO-incompatible heart transplant in infants: a UNOS database review. Ann Thorac Surg 2021;112:589-94. [Crossref] [PubMed]
- Urschel S, McCoy M, Cantor RS, et al. A current era analysis of ABO incompatible listing practice and impact on outcomes in young children requiring heart transplantation. J Heart Lung Transplant 2020;39:627-35. [Crossref] [PubMed]
- Jeyakanthan M, Meloncelli PJ, Zou L, et al. ABH-glycan microarray characterizes ABO subtype antibodies: fine specificity of immune tolerance after ABO-incompatible transplantation. Am J Transplant 2016;16:1548-58. [Crossref] [PubMed]
- Dean CL, Sullivan HC, Stowell SR, et al. Current state of transfusion practices for ABO-incompatible pediatric heart transplant patients in the United States and Canada. Transfusion 2018;58:2243-9. [Crossref] [PubMed]
- Costello JP, Carvajal HG, Abarbanell AM, et al. Surgical considerations in infant lung transplantation: challenges and opportunities. Am J Transplant 2021;21:15-20. [Crossref] [PubMed]
- Lally K, Kruse RL, Smetana H, et al. Isohemagglutinin titering performed on an automated solid-phase and hemagglutinin-based analyzer is comparable to results obtained by manual gel testing. Transfusion 2020;60:628-36. [Crossref] [PubMed]
- Lim YA, Kang SJ. Standardization of ABO antibody titer measurement at laboratories in Korea. Ann Lab Med 2014;34:456-62. [Crossref] [PubMed]
- AuBuchon JP, de Wildt-Eggen J, Dumont LJ, et al. Reducing the variation in performance of antibody titrations. Arch Pathol Lab Med 2008;132:1194-201. [Crossref] [PubMed]
- Bachegowda LS, Cheng YH, Long T, et al. Impact of uniform methods on interlaboratory antibody titration variability: antibody titration and uniform methods. Arch Pathol Lab Med 2017;141:131-8. [Crossref] [PubMed]
- Kobayashi T, Saito K. A series of surveys on assay for anti-A/B antibody by Japanese ABO-incompatible Transplantation Committee. Xenotransplantation 2006;13:136-40. [Crossref] [PubMed]
- Kahlyar H, Roxby D, Badrick T, et al. Challenges in antibody titration for ABO-incompatible renal transplantation. Vox Sang 2022;117:109-18. [Crossref] [PubMed]
- Bentall A, R, Barnett AN, Braitch M, et al. Clinical outcomes with ABO antibody titer variability in a multicenter study of ABO-incompatible kidney transplantation in the United Kingdom. Transfusion 2016;56:2668-79. [Crossref] [PubMed]
- Shirey RS, Cai W, Montgomery RA, et al. Streamlining ABO antibody titrations for monitoring ABO-incompatible kidney transplants. Transfusion 2010;50:631-4. [Crossref] [PubMed]
- Adkins BD, Arnold Egloff SA, Fahey-Ahrndt K, et al. An exploration of the advantages of automated titration testing: low inter-instrument variability and equivalent accuracy for ABO and non-ABO antibody titres relative to tube testing. Vox Sang 2020;115:314-22. [Crossref] [PubMed]
- Shim H, Hwang JH, Kang SJ, et al. Comparison of ABO isoagglutinin titres by three different methods: tube haemagglutination, micro-column agglutination and automated immunohematology analyzer based on erythrocyte-magnetized technology. Vox Sang 2020;115:233-40. [Crossref] [PubMed]
- Stussi G, Huggel K, Lutz HU, et al. Isotype-specific detection of ABO blood group antibodies using a novel flow cytometric method. Br J Haematol 2005;130:954-63. [Crossref] [PubMed]
- Tanabe K. Interinstitutional variation in the measurement of anti-A/B antibodies: the Japanese ABO-Incompatible Transplantation Committee survey. Transplantation 2007;84:S13-6. [Crossref] [PubMed]
- Valli PV, Puga Yung G, Fehr T, et al. Changes of circulating antibody levels induced by ABO antibody adsorption for ABO-incompatible kidney transplantation. Am J Transplant 2009;9:1072-80. [Crossref] [PubMed]
- Daniels G. Human blood groups. 3rd ed. Oxford: Wiley-Blackwell, 2013.
- Jeyakanthan M, Tao K, Zou L, et al. Chemical basis for qualitative and quantitative differences between ABO blood groups and subgroups: implications for organ transplantation. Am J Transplant 2015;15:2602-15. [Crossref] [PubMed]
- Holgersson J, Jovall PA, Samuelsson BE, et al. Blood group type glycosphingolipids of human kidneys. Structural characterization of extended globo-series compounds. Glycoconj J 1991;8:424-33. [Crossref] [PubMed]
- Holgersson J, Rydberg L, Breimer ME. Molecular deciphering of the ABO system as a basis for novel diagnostics and therapeutics in ABO incompatible transplantation. Int Rev Immunol 2014;33:174-94. [Crossref] [PubMed]
- Ravn V, Dabelsteen E. Tissue distribution of histo-blood group antigens. APMIS 2000;108:1-28. [Crossref] [PubMed]
- Perry H, Bovin N, Henry S. A standardized kodecyte method to quantify ABO antibodies in undiluted plasma of patients before ABO-incompatible kidney transplantation. Transfusion 2019;59:2131-40. [Crossref] [PubMed]
- Lindberg L, Theinert K, Liu J, et al. Adsorption of chain type-specific ABO antibodies on Sepharose-linked A and B tetrasaccharides. Transfusion 2012;52:2356-67. [Crossref] [PubMed]
- Padmanabhan A, Connelly-Smith L, Aqui N, et al. Guidelines on the use of therapeutic apheresis in clinical practice - evidence-based approach from the Writing Committee of the American Society for Apheresis: The Eighth Special Issue. J Clin Apher 2019;34:171-354. [Crossref] [PubMed]
- Abbes S, Metjian A, Gray A, et al. Human leukocyte antigen sensitization in solid organ transplantation: a primer on terminology, testing, and clinical significance for the apheresis practitioner. Ther Apher Dial 2017;21:441-50. [Crossref] [PubMed]
- Simmons SC, Adamski J, Berg M, et al. The apheresis management of patients undergoing transplantation: a concise review. Transfusion 2019;59:1863-9. [Crossref] [PubMed]
- Tamain M, Sayegh J, Lionet A, et al. Extracorporeal photopheresis for the treatment of graft rejection in 33 adult kidney transplant recipients. Transfus Apher Sci 2019;58:515-24. [Crossref] [PubMed]
- Schneiderman J. Extracorporeal photopheresis: cellular therapy for the treatment of acute and chronic graft-versus-host disease. Hematology Am Soc Hematol Educ Program 2017;2017:639-44. [Crossref] [PubMed]
Cite this article as: Ramsey G. Blood banking in solid organ transplantation. Ann Blood 2022;7:15.


