
The importance of patient blood management for patients, providers and the public
Introduction
Background
Almost every clinical specialty employs blood transfusion at some point for patient care. The traditional model of a transfusion evokes an image of a patient lying in a bed and the physician standing or sitting by the bedside explaining the risks and benefits. The provider has decided to transfuse based on the patient’s described symptoms and observed signs of hemodynamic instability, or severe life-threatening cytopenia. The blood component is then ordered and transfused by a nurse or physician who remains nearby to closely monitor the patient for a reaction. The parties involved appear to be only the patient, the prescriber, and the transfusionist.
In reality, the process is more complex, involving many stakeholders not only within the healthcare system but also in society at large because of the need to procure blood products from volunteer donors. Ironically, the field of “transfusion medicine” has mainly been under the purview of specialists who do not even appear in the traditional model described above. For many years, these blood banking and transfusion medicine specialists were tasked with overseeing the transfusion process starting from a focus on the safety of the donors to ensuring the purity and potency of the blood components on their journey to the bedside. This also included screening for proper ordering based on sound indications as well as monitoring the safety of the patients during and after the transfusion procedure through investigation of transfusion reactions when they occur. However, due to increasing appreciation of the risks of transfusion, scarcity of the blood supply, the experience of patients for whom blood is not an option, and the complexity of the process, the concept of “Patient Blood Management (PBM)” was born.
An expert group representing PBM organizations, from the International Foundation for Patient Blood Management (IFPBM), the Network for the Advancement of Patient Blood Management, Haemostasis and Thrombosis (NATA), the Society for the Advancement of Patient Blood Management (SABM), the Western Australia Patient Blood Management (WAPBM) Group, and ONTraC (Ontario Transfusion Coordinators) program recently convened and developed this PBM definition: “Patient blood management is a patient-centered, systematic, evidence-based approach to improve patient outcomes by managing and preserving a patient’s blood while promoting patient safety and empowerment.” (1). In practice, satisfying this definition requires a multi-disciplinary and coordinated approach to try to avoid blood transfusion. If a transfusion is needed it is essential to maximize the benefit and safety for the patient.
Rational and knowledge gap
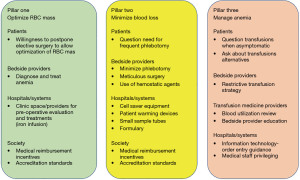
Regarding the decision to transfuse described in the first paragraph, there is now a greater appreciation of interventions needed before the clinician approaches the bedside to obtain consent to transfuse. These interventions cannot be accomplished by any individual practitioner and require infrastructure and investment in processes outside of the scope of a single hospital department. Although a “three pillars concept of PBM” has been described (2), there is insufficient appreciation that the essential components are under the primary control of different practitioners in the health care system (Figure 1). The outpatient practitioners of pillar 1 who should be diagnosing pre-operative anemia and the practitioners of pillar 2 who should be minimizing blood loss in the OR are often not the same practitioner at the bedside on the ward of pillar 3, wondering if the anemic and possibly lightheaded patient can be discharged home without a transfusion.
Objective
This paper will describe the roles and responsibilities of the various stakeholders in PBM. By focusing on the stakeholders rather than the overall process or program, the importance of PBM will become more tangible to all parties, and implementation a more achievable goal.
Centering the patient
It is intentional that this article begins with the patient. It is deliberate that even the term “Patient Blood Management” prioritizes the word “patient”. The primary focus of PBM programs is the management of the patient’s blood, not the blood stored at the blood center. The priority is to manage the patient’s blood to optimize the patient’s well-being and ultimately eliminate or drastically reduce the need for allogeneic blood products. The proposed global definition of PBM emphasizes the critical role of informed choice centered on the patient’s values and preferences. It also emphasizes evidence-based treatments focused on documented patient needs. In a situation in which an individual has a planned treatment that may include blood loss, it is important for the clinical team to assess the patient’s blood status. Screening for anemia in advance of any invasive procedures is paramount. The more in advance, the screening is performed, the more time the intervention (if needed) can be planned and executed. The patient should be included and informed of plan options, the plan’s goal, and the expected outcome of each option.
As a specific sample, anemia and iron deficiency are recognized as serious global health issues. In the most recent Global Burden of Disease study, iron deficiency anemia is amongst the top five causes of years lived with disability and a top ten diseases in prevalence estimated to affect 1.24 billion people (3). While many PBM efforts have been focused on improving decisions made around the decision to transfuse (what product, what amount, and when), a well-executed PBM framework will address iron deficiency anemia and other common patient conditions that can be treated without an allogeneic blood transfusion. The patient populations that would benefit from these efforts are wide and include inpatients and outpatients, medical and surgical patients, pregnant women, and patients of all ages from pediatric to the elderly.
In promulgating the three-pillar concept of PBM James Isbister noted: “With greater empowerment of patients by involvement in determining their clinical management, there are complex issues surrounding consent as to what information about PBM and blood transfusion should be provided, how should it be communicated and documented to confirm that it has been validly achieved.” (2). This point raises a provocative question. “In the absence of patient awareness of the concept of PBM, can it be said every patient has granted ‘informed consent’ for a blood transfusion?” If the evidence supports the superiority of PBM over transfusion, the answer is “no,” hence patients need to be educated about the importance of PBM, and the use of PBM should serve as an indicator of quality.
Bedside health care providers
By incorporating PBM into their daily clinical practice, healthcare providers not only have the opportunity to deliver more patient-centered care and to improve patient outcomes but also to save costs for the hospital (4-9). Provider-level PBM measures begin with the identification of those who are engaged and committed to supporting a PBM program. These are those individuals who serve as local champions to promote the importance of PBM across disciplines and drive the various PBM initiatives in collaboration with a multidisciplinary team of professionals.
The multidisciplinary nature of PBM is of paramount importance for building a comprehensive system that assists the health care providers with their decision-making related to managing their patient’s blood. Development of patient-centered evidence-based guidelines along with policies for managing anemia and optimizing hemostasis, provider education and information technology (IT) support for interactive communication with providers, data collection and analyzing outcomes are some of the key components in the success of a PBM program (4,7,8).
Healthcare provider vigilance in addressing the three PBM pillars is associated with a reduction in the use of allogeneic blood components and improved patient outcomes (5). Identification of patients at increased risk for anemia and coagulopathy, limiting phlebotomy and volume of sampling, incorporation of meticulous surgical/anesthesia techniques and devices (i.e., cell saver), viscoelastic point of care testing for assessment of hemostasis/coagulopathy, adherence to evidence-based transfusion guidelines/restrictive transfusion practices, and use of pharmaceutical therapy such as oral/IV iron therapy for the treatment of anemia and antifibrinolytics, topical hemostatic agents, prothrombin complex concentrate, and other clotting factors for managing blood loss and/or coagulopathy are some of the effective strategies for the healthcare providers to incorporate into their clinical practice (4,5,7).
As many providers are unfamiliar with the latest PBM best practices and guidelines, education across various disciplines is essential for their buy-in, compliance with guidelines, and raising awareness of the PBM program. Provider education should address staff physicians, residents/fellows, nurses, advanced care providers, and others who can influence the decisions related to transfusions and preserving the patient’s blood. Education can be achieved through various offerings such as grand round presentations, in-services, computerized educational modules, and social media platforms. Emphasis on findings from randomized controlled trials supporting restrictive transfusions, incorporation of Choosing Wisely recommendations by SABM, the Association for the Advancement of Blood and Biotherapies (AABB), and other professional organizations, and other relevant PBM publications raise provider awareness of current data in PBM. These resources are effective measures to help influence providers to change their behavior, at least until data can be obtained from their hospital or hospital system (8-12) that show these practices are effective here as well. Computerized provider order entry with clinical decision support that includes educational messaging and interactive best practice advisories and initiatives such as the single unit transfusion campaign for red blood cells (RBCs) and platelets provide additional provider education on PBM best practices (7).
Once the providers are educated on PBM best practices and guidelines, it is important to develop organizational dashboards and monitor blood utilization and other PBM metrics for compliance with periodic feedback to providers regarding their practices. Peer-to-peer comparisons of compliance with evidence-based practices have been shown to be an effective strategy to further encourage providers to adhere to PBM guidelines and reduce inappropriate transfusions. PBM metrics and compliance data should be regularly reported to committees that perform ongoing monitoring and follow-up of PBM practices (6,8,9).
Transfusion medicine and transfusion safety specialists
Because of close affiliation with blood collection centers, blood banks, or the transfusion service portion of a hospital laboratory where blood components are located, transfusion specialists traditionally are viewed to be blood component centered. However, when transfusion medicine or transfusion safety specialists are charged with investigating a transfusion event, such as a reaction or the indication to transfuse the focus becomes patient-centered. But after the investigation is completed, the event is often simply entered into a data set to trend usage, types of reactions, or adherence to transfusion thresholds to provide direction to programmatic interventions. This is not adequate with a robust PBM program. The analysis should not simply focus on the transfusion event, but also whether the principles of PBM were adhered to in the patient encounter. For example, the third pillar or principle of PBM involves “use of restrictive transfusion strategies” (2), or “evidence-based transfusion strategies” (13) and includes as a fundamental corollary “avoiding or minimizing unnecessary allogeneic blood transfusions” (2). Every transfusion can then reasonably be questioned as a possible failure of adherence to all PBM principles. Long before PBM came into existence, hospitals had “transfusion review committees” or “blood utilization review committees” with the same underlying principle that transfusions are worth questioning (14). However, instead of the traditional transfusion review committee paradigm of looking at a possible failure to adhere to transfusion indication guidelines, the review can consider whether there was a failure to diagnose iron deficiency anemia pre-operatively. In other words, acute symptomatic anemia may be an appropriate indication to transfuse, but the patient may not have arrived at that situation if there was adherence to the first two pillars of PBM (1st maximizing total RBC mass and 2nd minimizing blood loss). It’s not just the hemoglobin value and symptoms just before the post-operative transfusion that matters, but also the pre-operative hemoglobin and blood loss documented in the operative note.
Hospitals/hospital systems with a focus on the United States
While PBM has demonstrated improved outcomes for patients, hospitals and healthcare systems will need to demonstrate to themselves that the investment in the implementation will be of a net benefit. This is viewed from a United States (US) perspective where the independent operation of the blood centers and hospitals lead to budgeting concerns. The data presented by the US-based Joint Commission with the American Medical Association in 2012 targeted blood transfusion as a top overused procedure (15). By “right sizing” the hospital transfusion practice, opportunities to save on blood costs, improve blood inventory and avoid adverse events can be realized. With a good analysis of historic and current blood use and transfusion-related activities, hospital leadership can be shown the numerous advantages of initiating PBM activities.
The easiest math on benefits of PBM will be on cost savings of transfusing fewer blood products. A hospital’s blood budget can be a large line item, and inpatient transfusions, in particular, will be difficult to recover expenses. One group calculated that the total cost of a single transfusion is upward of $1000 US dollars (USD) when indirect costs are included (16), while in Europe the estimate of a two-unit RBC transfusion was EU877 (17). When just the blood products are considered, the costs to the hospitals also continue to rise as the blood centers must balance the declining number of transfusions against the increased mandatory transfusion-transmitted disease screening and quality control required for each donation. Implementation of PBM strategies for a district in Australia saw a 41% decrease in blood product utilization, translating to savings of Australian dollars $18,507,092 (USD $18,078,258) (6).
Resource scarcity is another aspect of challenge at the hospital level. Unprecedented blood shortages occurred in the US in the second half of 2021, leaving hospitals and hospital systems scrambling to maintain patient care (18). The most recent National Blood Collection and Utilization Survey from 2019 suggested this very situation as it saw a narrowing in the gap between blood collected versus blood transfused due to decreased collections and stable or even increased utilization of some blood components (19). Not having enough blood inventory on the shelf may lead to the cancellation of surgery, delay of needed transfusions, and worse patient outcomes. Blood ordering and utilization reviews as part of a PBM program will also identify overordering by reviewing crossmatch to transfusion or preparation to transfusion ratios as well as blood wastage. Once the trend is recognized, the PBM team can implement strategies to prevent wastage. By implementing PBM techniques, the hospital system will have a reduced overall need for transfusion and the shared vocabulary of PBM will provide the communication tools for rapid practice changes when faced with future critical inventory shortages.
Transfusion reactions are an often-underappreciated source of harm and cost at the administrative or bedside provider level. Acute transfusion reactions, due to immune and non-immune causes, lead to increased length of stay, higher acuity of care, and even permanent injury/mortality to the patient. The current estimated rate of serious transfusion reactions is 1 in 6,224 transfusions according to the National Healthcare Safety Network Hemovigilance Module (20). For a hospital, increased length of stay and higher care acuity negatively affect hospital flow. Particularly in the COVID era, multifactorial staffing shortages have led to fewer available hospital beds, making good patient flow through the hospital more critical (21). A 2019 study in surgery patients found that implementation of PBM practices did reduce hospital length of stay (22). One Canadian study, performed prior to the COVID era, found that 24% of RBC transfusions in their audits were not appropriate according to the institution’s transfusion guidelines (23). While preventing all transfusion reactions is impossible, restricting transfusion to those who truly need it and transfusing appropriately will avoid potentially avoidable adverse events that require higher care acuity and lead to increased morbidity and even mortality.
To support the initiation of PBM, which involves multidisciplinary acceptance and resource investment by the health system, several groups have put forth certifications to provide the steps and external incentives for implementation. Conducting regular blood utilization audits (retrospective as well as prospective) forms an integral part of the PBM program, and it helps in improving the quality standards of the hospital (24). A recent international survey addressing barriers and steps to advance PBM programs identified provider buy-in and education as a significant piece of success (8). In the US, The Joint Commission with AABB now has a hospital certification that has been developed to standardize and strengthen PBM programs (25).
Benchmarking against similar hospitals can aid in evaluating opportunities at a care service level and across similar diagnoses. Engaging IT resources early is an important step in tracking and trending. Metrics may include transfusions per patient, percent patient encounters receiving transfusion, and blood wastage rates. Following a familiar path of quality assurance in healthcare, data flow is established, goals are set, and quality improvement techniques are implemented.
Government/society at large
The PBM program helps not only the hospitals to run transfusion services efficiently, but the benefits extend to the society and general population as well. It has assumed a much bigger role in the backdrop of the ongoing COVID-19 pandemic. The severe shortage of blood products during the start of the pandemic was evident when the American Red Cross (ARC) and US Surgeon General had to appeal to all healthy young individuals in March 2020 to donate blood in the time of crisis (26). Since then, much focus has shifted in many facilities to implementing a robust PBM program for optimal utilization of the limited blood supply. The scarcity of blood has persisted throughout the pandemic as the AABB, America’s Blood Centers, and ARC again issued a joint statement in January 2022 to urge eligible, healthy individuals to contact their local blood center and make an appointment to donate blood (27). There is a limited healthy donor pool in any city or region and judicious use of blood ensures better availability for all the hospitals and patients in that area. As more organizations start to follow the tenets of PBM, it is hoped that more blood products will become available for those who need them.
Implementing PBM also helps in better management of regulatory issues associated with the transfusion services. It may further assist in the better settlement of insurance claims. A well-implemented PBM program can help in reducing the number of hospital days, as documented by a study in Western Australia, which showed that hospital stays were reduced by almost 70,000 days over 5 years (6). PBM has also contributed to the detection and early treatment of anemia for a large number of patients who might have remained undiagnosed and untreated otherwise (28).
Both top-down (from government and/or system leadership and formed policies) and bottom-up (individual providers, department, or hospital level) can be successful for initiation. Simultaneous implementation of both has been advised for better outcomes (8). National information campaigns and patient advocacy groups can help in spreading awareness about the importance of PBM among the general population. As these measures become more widespread over time, a larger section of society will benefit from them.
Metrics
Metrics from a 3-hospital 521 bed-system in the US are available. For appropriateness of allogeneic transfusion overall compliance of RBC, platelet and plasma transfusion thresholds on average yearly [2019, 2020] was: RBC’s 99.8%, platelets 99.4%, plasma 99.8%. RBC wastage remained low (0.74% 2019, 0.79% 2020).
Showing that PBM is a constant challenge, in 2019 the costs of all blood products increased by $20,937.33 USD as compared to 2018. In 2020, through educational efforts, the cost savings was $124,856.70 USD compared to 2019.
Regarding single unit transfusion of RBCs, this was 62.25% [2019], 63.75% [2020], and 72.00% [2021], and surpassed the target goal of 60% (which was increased to 70% for 2022). The rate at which patients in the hospital were transfused was 52.82% in 2014 when the PBM program was started and had decreased to 32.44% by 2020 (25).
Strengths and limitations
Strengths of this manuscript are that it was written by a group of subject matter experts in PBM. Weaknesses of the paper include that the manuscript has a focus on PBM in North America and in high-income countries. A PBM program and challenges faced by low and middle-income countries may be different from those discussed in this manuscript.
Conclusions
Successful implementation of a PBM program requires the collaboration of dedicated healthcare professionals and an extensive team of partners. These include quality officers, IT specialists, bedside caregivers, and organizational leadership who work synergistically towards implementing and supporting strategies that preserve patients’ blood, ultimately minimizing the need for transfusions.
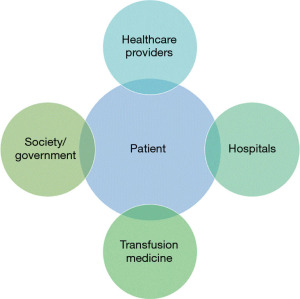
Patients, healthcare providers, transfusion specialists, hospital and healthcare system administrators, and community citizens at large should be aware of the importance of the PBM approach to care. It is important for patients to know that blood transfusions can potentially be avoided or minimized when seeking care that has traditionally required them. It is important for healthcare providers to render the best possible care to their patients. It is important for transfusion medicine and transfusion safety specialists to move beyond the traditional transfusion /blood utilization review paradigm of questioning individual provider decisions at the moment of transfusion and recognize the benefit of pre-transfusion anemia treatment. It is important for hospitals and hospital systems to recognize the cost savings that will result from supporting some simple upfront infrastructure support needed for individual healthcare providers to implement a PBM program approach to care. On a societal level, it may be necessary to create reimbursement incentives or public information campaigns to enable more widespread and robust PBM programs to improve population health as well as protecting the community resource of the blood supply (Figure 2).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Blood for the series “Patient Blood Management’s Role in Current Healthcare Environment”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aob.amegroups.com/article/view/10.21037/aob-22-39/coif). The series “Patient Blood Management’s Role in Current Healthcare Environment” was commissioned by the editorial office without any funding or sponsorship. JP is a subinvestigator on a blood product study that Cerus is funding. JP is also on a College of American Pathologists committee the plans meeting curriculum and they pay travel costs for meetings, and JP consulted with Secure Transfusion Services one time on platelet utilization trends in 2021, prior to working on this manuscript, so there is no conflicts of interest that relate to this manuscript. RG served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shander A, Hardy JF, Ozawa S, et al. A Global Definition of Patient Blood Management. Anesth Analg 2022;135:476-88. [Crossref] [PubMed]
- Isbister JP. The three-pillar matrix of patient blood management. ISBT Sci Ser 2015;10:286-94. [Crossref]
- Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1211-59. [Crossref] [PubMed]
- Meybohm P, Herrmann E, Steinbicker AU, et al. Patient Blood Management is Associated With a Substantial Reduction of Red Blood Cell Utilization and Safe for Patient's Outcome: A Prospective, Multicenter Cohort Study With a Noninferiority Design. Ann Surg 2016;264:203-11. [Crossref] [PubMed]
- Althoff FC, Neb H, Herrmann E, et al. Multimodal Patient Blood Management Program Based on a Three-pillar Strategy: A Systematic Review and Meta-analysis. Ann Surg 2019;269:794-804. [Crossref] [PubMed]
- Leahy MF, Hofmann A, Towler S, et al. Improved outcomes and reduced costs associated with a health-system-wide patient blood management program: a retrospective observational study in four major adult tertiary-care hospitals. Transfusion 2017;57:1347-58. [Crossref] [PubMed]
- Frank SM, Thakkar RN, Podlasek SJ, et al. Implementing a Health System-wide Patient Blood Management Program with a Clinical Community Approach. Anesthesiology 2017;127:754-64. [Crossref] [PubMed]
- Hofmann A, Spahn DR, Holtorf AP, et al. Making patient blood management the new norm(al) as experienced by implementors in diverse countries. BMC Health Serv Res 2021;21:634. [Crossref] [PubMed]
- Mehra T, Seifert B, Bravo-Reiter S, et al. Implementation of a patient blood management monitoring and feedback program significantly reduces transfusions and costs. Transfusion 2015;55:2807-15. [Crossref] [PubMed]
- Callum JL, Waters JH, Shaz BH, et al. The AABB recommendations for the Choosing Wisely campaign of the American Board of Internal Medicine. Transfusion 2014;54:2344-52. [Crossref] [PubMed]
- ABIM Foundation. Five Things Physicians and Patients Should Question. 2022. Cited 2022 Jul 27. Available online: https://www.aabb.org/docs/default-source/default-document-library/resources/choosing-wisely-five-things-physicians-and-patients-should-question.pdf
- Burns CD, Brown JP, Corwin HL, et al. Special Report From the Society for the Advancement of Blood Management: The Choosing Wisely Campaign. Anesth Analg 2019;129:1381-6. [Crossref] [PubMed]
- Goodnough LT, Shander A. Patient blood management. Anesthesiology 2012;116:1367-76. [Crossref] [PubMed]
- Walz DV. An effective hospital transfusion committee. JAMA 1964;189:660-2. [Crossref] [PubMed]
- Proceedings from the National Summit on Overuse. September 24, 2012. Accessed 30 March 2023. Available online: https://www.parsemus.org/wp-content/uploads/2015/06/AMA-National_Summit_Overuse.pdf
- Shander A, Hofmann A, Ozawa S, et al. Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion 2010;50:753-65. [Crossref] [PubMed]
- Abraham I, Sun D. The cost of blood transfusion in Western Europe as estimated from six studies. Transfusion 2012;52:1983-8. [Crossref] [PubMed]
- Rosen NS. Severe national blood shortage may force doctors to augment patient care, officials say. ABC news June 20, 2021. Accessed 20 June 2022. Available online: https://abcnews.go.com/Health/severe-national-blood-shortage-force-doctors-augment-patient/story?id=78354725
- Jones JM, Sapiano MRP, Mowla S, et al. Has the trend of declining blood transfusions in the United States ended? Findings of the 2019 National Blood Collection and Utilization Survey. Transfusion 2021;61:S1-S10. [Crossref] [PubMed]
- Kracalik I, Mowla S, Basavaraju SV, et al. Transfusion-related adverse reactions: Data from the National Healthcare Safety Network Hemovigilance Module - United States, 2013-2018. Transfusion 2021;61:1424-34. [Crossref] [PubMed]
- US Department of Health and Human Services. Impact of the COVID-19 Pandemic on the Hospital and Outpatient Clinician Workforce. Cited 2022 Aug 22. Available online: https://aspe.hhs.gov/sites/default/files/documents/9cc72124abd9ea25d58a22c7692dccb6/aspe-covid-workforce-report.pdf
- Faulds J, Whately-Smith C, Clarke K. Transfusion requirement and length of stay of anaemic surgical patients associated with a patient blood management service: a single-Centre retrospective study. Transfus Med 2019;29:311-8. [Crossref] [PubMed]
- Spradbrow J, Cohen R, Lin Y, et al. Evaluating appropriate red blood cell transfusions: a quality audit at 10 Ontario hospitals to determine the optimal measure for assessing appropriateness. Transfusion 2016;56:2466-76. [Crossref] [PubMed]
- Stanworth SJ, Lorencatto F, Gould N, et al. Can we do better? Bridging the research to practice gap in patient blood management–optimizing ‘audit & feedback’ and the challenges of undertaking a national cluster-randomized controlled trial. ISBT Sci Ser 2019;14:129-35. [Crossref]
- Gammon RR, Blanton K, Gilstad C, et al. How do we obtain and maintain patient blood management certification? Transfusion 2022;62:1483-94. [Crossref] [PubMed]
- Stephenson J. Canceled Blood Drives, Social Distancing Cause Nationwide Blood Shortages. JAMA Health Forum 2020;1:e200380. [Crossref] [PubMed]
- Joint Statement: Blood Donors Urgently Needed During National Blood Donor Month and Throughout the Winter. Cited 2022 Jan 10. Available online: https://www.redcross.org/about-us/news-and-events/press-release/2022/joint-statement-blood-donors-urgently-needed.html
- Shander A, Van Aken H, Colomina MJ, et al. Patient blood management in Europe. Br J Anaesth 2012;109:55-68. [Crossref] [PubMed]
Cite this article as: Gilstad CW, Poisson J, Dubey R, Shariatmadar S, Jorgenson M, Gammon R. The importance of patient blood management for patients, providers and the public. Ann Blood 2023;8:34.


