
Frequencies of ABO and RhD blood groups among blood donors in Hong Kong
Introduction
Since the discovery of ABO blood group from the presence of A and B antigens on the surface of red blood by Karl Landsteiner in 1901, our understanding of human blood groups is much expanded. To date, the International Society of Blood Transfusion has listed 44 blood group systems with more than 354 red blood cell (RBC) antigens (1). Some of them have been showed to be of clinical and transfusion significances (2-4). Of them, ABO and Rh blood groups are the most clinically important in blood transfusion. For example, as little as 0.03 mL of Rhesus D (RhD) positive RBCs can induce the anti-D formation in an RhD negative adult and anti-D could cause serious morbidities or even mortalities in hemolytic disease of fetus and newborn (HDFN) (5,6). Therefore, to ensure safe clinical transfusion practice, compatibility between the donor and recipient is crucial to prevent any adverse transfusion event (in particular acute and delayed haemolytic transfusion reaction). Moreover, not surprisingly, blood group distribution is not only different and distinctive between population groups, but also changing time to time in the same region with population mobility (7-15). An updated knowledge of their distribution among local population would be extremely helpful in blood donor recruitment and provision of adequate blood supply for clinical transfusion.
Being an international city with a lot of travel activities and also many non-Chinese either working or studying in Hong Kong, though majority of local citizens remains Chinese, changes in other racial population are not uncommon as reflected in the regular government census reports (16). Therefore, there remains a lack of published data nor regular update describing the blood group distribution of the local population. Therefore, the aim of this study is to determine the phenotypic frequencies of ABO and RhD blood groups in Hong Kong. Apart from the application in clinical transfusion, the data generated would be of use to the blood transfusion service (BTS) in developing a better and rational strategy for blood donor recruitment, blood collection and transfusion demand management.
Materials and methods
Subjects
A retrospective study was conducted at the Hong Kong Red Cross Blood Transfusion Service for a 10-year period from 1 January 2011 to 31 December 2020. The ABO and RhD phenotyping results of 164,095 and 2,996 Chinese and non-Chinese donors (NCD), respectively were retrieved from the blood bank computing system for analysis. They were all voluntary non remunerated first-time blood donors of age between 16 and 65, who were accepted to blood donation after passing through the prevailing donor eligibility criteria. No previous or repeated donors were included in the study. Prospective donors were allowed to donate blood in Hong Kong provided that they fulfilled the donor selection criteria and have Hong Kong Identity Card or travel document such as passport and with contactable information including telephone and address. NCD defined in this study consisted of White, Indian, Indonesian and Filipino and their number of blood donors had to be more than 100 cumulatively during the studied period. Their ethnicities were determined at pre donation health history enquiries.
Blood group typing methods
Locally, ABO and RhD groups of donors were determined using PK 7300/7400 (Beckman Coulter, USA), a fully automated and high throughput system using microplate technique and conventional tube method if there were doubt or inconsistencies in forward and reverse grouping. All the reactions were observed macroscopically and interpreted by agglutination. Positive and negative controls cells were used as quality controls per organizational standard operating procedures. In addition, weak D test would be performed on all first-time donors with D negative finding on PK7300/7400. All weak D positive would then be labelled as RhD positive. However, D elution (DEL) test is not a routine procedure for weak D negative donors, particularly on phenotype, rr, donors.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The data for this study was day to day operational information of the organization and involved no individual information but aggregated from the computing system. Therefore, no ethical approval nor informed consent was required.
Results
A total of 167,091 ABO and RhD records from 164,095 Chinese donors and 2,996 NCD aged 16 to 70 years were retrieved for the study period. Table 1 summarized their gender and age. Of them, there were 78,100 or 46.7% male (77,285 being Chinese donors and 815 as NCD) and 88,991 or 53.3% female (86,810 in Chinese donors and 2,181 as NCD); 93,093 (56.7%) were under the age of 39 years with age group of 20–29 years (28.3%) being the largest in Chinese donors. On the other hand, donors’ age of 40–49 years was observed as the major group in other populations. While there was no gender difference in Chinese, White and Indian donors, female was predominant among Indonesian and Filipino population which was likely due to their occupations in Hong Kong.
Table 1
| Demographics | Chinese (n=164,095), n (%) | White (n=616), n (%) | Indian (n=523), n (%) | Indonesian (n=1,404), n (%) | Filipino (n=453), n (%) |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 77,285 (47.1) | 319 (51.8) | 304 (58.1) | 93 (6.6) | 99 (21.9) |
| Female | 86,810 (52.9) | 297 (48.2) | 219 (41.9) | 1,311 (93.4) | 354 (78.1) |
| Age range (years) | |||||
| <20 | 506 (0.3) | 5 (0.8) | 12 (2.3) | 4 (0.3) | 4 (0.9) |
| 20–29 | 46,512 (28.3) | 117 (19.0) | 126 (24.1) | 67 (4.8) | 53 (11.7) |
| 30–39 | 46,075 (28.1) | 116 (18.8) | 92 (17.6) | 616 (43.9) | 140 (30.9) |
| 40–49 | 35,363 (21.6) | 149 (24.2) | 171 (32.7) | 614 (43.7) | 165 (36.4) |
| 50–59 | 24,598 (15.0) | 145 (23.5) | 87 (16.6) | 89 (6.3) | 67 (14.8) |
| ≥60 | 11,041 (6.7) | 84 (13.6) | 35 (6.7) | 14 (1.0) | 24 (5.3) |
NCD, non-Chinese donors.
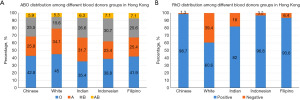
The distribution of ABO and RhD was summarized in Table 2 and Figure 1. Locally, the most commonly observed ABO blood group was group O ranging from 35.4% to 45.0% with 42.8% and 45.0% in Chinese and White donors respectively. It was followed by group A with a range of 23.4% to 34.1%; group B from 15.6% to 30.7% and lastly AB from 5.3% to 7.1%. Of interest, group A and B were about the same in Chinese and Filipino donors but more A were seen in White (34.1% vs. 15.6%) and Indian (31.7% vs. 26.6%) donors. For RhD, majority of the local donors were RhD positive—being 98.7% in Chinese, 96.8% in Indonesian and 93.6% for those come from Filipinos. However, a higher percentage of RhD negative was found in Indian (18.0%) and White (39.4%) donors.
Table 2
| ABO and RhD status | Chinese (n=164,095), n (%) |
White (n=616), n (%) | Indian (n=523), n (%) | Indonesian (n=1,404), n (%) |
Filipino (n=453), n (%) |
|---|---|---|---|---|---|
| RhD + | |||||
| A | 41,475 (25.3) | 123 (20.0) | 141 (27.0) | 317 (22.6) | 109 (24.1) |
| B | 41,542 (25.3) | 63 (10.2) | 107 (20.5) | 423 (30.1) | 108 (23.8) |
| O | 69,356 (42.3) | 163 (26.5) | 153 (29.3) | 522 (37.2) | 177 (39.1) |
| AB | 9,581 (5.8) | 24 (3.9) | 28 (5.4) | 97 (6.9) | 30 (6.6) |
| RhD − | |||||
| A | 827 (0.5) | 87 (14.1) | 25 (4.8) | 12 (0.9) | 6 (1.3) |
| B | 295 (0.2) | 33 (5.4) | 32 (6.1) | 8 (0.6) | 8 (1.8) |
| O | 913 (0.6) | 114 (18.5) | 32 (6.1) | 22 (1.6) | 13 (2.9) |
| AB | 106 (0.1) | 9 (1.5) | 5 (1.0) | 3 (0.2) | 2 (0.4) |
RhD, Rhesus D; NCD, non-Chinese donors.
Discussion
It is observed in this study that group O (42.8%) is the most common ABO group of Hong Kong Chinese, followed by group A (25.8%), group B (25.5%) while group AB (5.9%) is the least common (Table 2). When comparing to the findings in other studies on Chinese population, though group O is the commonest, variations in the ABO frequency were often seen with group A ranged from 25.2% to 30.7% and group B from 26.4% to 30.8% (14,17-19). With at least 18.5% world population being Chinese, 56 ethnic groups in China and years of population movement, this variation is not unexpected. On the other hand, the ABO blood group prevalence of White population in the present study was similar to that reported in Australia and United States (US) (8,13,20); with group A White donors about two times that of group B (34% vs. 16%). However, an even higher prevalence of group A (43%) which is close to that of group O (44%) has been reported in some studies about the White population in United States (20).
For the RhD status, the present study confirmed a high frequency (98.7%) of RhD positive among Chinese donors in Hong Kong, which is in agreement with the population of Indonesian, Filipino in HK and Chinese in Mainland. Up to 6% of Filipino and 3% of Indonesian donors were RhD negative. However, this high prevalence of RhD positive status in Hong Kong Chinese is at variance with the Indian (82% RhD positive versus 18% RhD negative). In fact, the RhD negative prevalence among different White population in US can vary from 15% to 39% (20). The above information would be extremely useful for the BTS in maintaining the RhD negative blood supply or blood inventory. It is because although majority of local population are RhD positive, when a demand for RhD negative blood for example for reproductive women is needed, the BTS has to swiftly provide sufficient and appropriate blood units to ensure transfusion treatment could be fulfilled. Therefore, these donors should be encouraged to donate regular or be kept contactable by phone or email for blood donation. In fact, the BTS is maintaining a daily inventory of small number of liquid RhD negative blood units to meet the urgent transfusion need whereas a pool of RhD negative donors are retained and be readily available to donate when requested. This kind of arrangement is frequently adopted in BTS who serves mostly RhD positive population. Nevertheless, the BTS should always monitor and demand and supply balance and proactively communicates with donors to come back.
In conclusion, this study provides an updated frequencies of ABO and RhD positive blood groups among donors in Hong Kong. The distribution allows the BTS to work proactively in securing a stable and sufficient supply of right blood groups in meeting clinical need. The difference in their prevalence among Chinese donors and NCDs population would also a useful reference guideline for hospital blood banks and clinical staff in the management of their patients. Last but not the least, with more population migration and changes, the BTS should not only handle the frequencies of ABO and RHD blood group among blood donors, but also need to work the prevalence of other blood groups, e.g., the prevalence of CcEe antigens in the population and patients in advance so that appropriate strategies be implemented to ensure the availability of suitably matched blood for clinical transfusion therapy.
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at https://aob.amegroups.com/article/view/10.21037/aob-23-6/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aob.amegroups.com/article/view/10.21037/aob-23-6/coif). CKL serves as an unpaid editorial board member of Annals of Blood from July 2022 to June 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The data for this study was day to day operational information of the organization and involved no individual information but aggregated from the computing system. Therefore, no ethical approval nor informed consent was required.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- International Society of Blood Transfusion Working Party on Red Cell Immunogenetics and Blood Group Terminology. 201 Table of blood group systems 2022 [updated 31/12/2022]. Available online: https://www.isbtweb.org/resource/tableofbloodgroupsystems.html. Last accessed 03/08/2023.
- Garratty G. What is a clinically significant antibody? ISBT Science Series 2012;7:54-7. [Crossref]
- Poole J, Daniels G. Blood group antibodies and their significance in transfusion medicine. Transfus Med Rev 2007;21:58-71. [Crossref] [PubMed]
- White J. Red cell antibodies – clinical significance or just noise? ISBT Science Series 2017;12:19-24. [Crossref]
- Jakobowicz R, Williams L, Silberman F. Immunization of Rh-negative volunteers by repeated injections of very small amounts of Rh-positive blood. Vox Sang 1972;23:376-81. [PubMed]
- Rh Blood Group System. In: Daniels G. Human Blood Groups (Second Edition). Oxford: Blackwell Science; 2002.
- Agarwal N, Thapliyal RM, Chatterjee K. Blood group phenotype frequencies in blood donors from a tertiary care hospital in north India. Blood Res 2013;48:51-4. [Crossref] [PubMed]
- Garratty G, Glynn SA, McEntire R, et al. ABO and Rh(D) phenotype frequencies of different racial/ethnic groups in the United States. Transfusion 2004;44:703-6. [Crossref] [PubMed]
- Hawkins BR, Simons MJ. Blood group genetic studies in an urban Chinese population. Hum Hered 1976;26:441-53. [Crossref] [PubMed]
- Jekarl DW, Yoo J, Lee S, et al. Blood group antigen and phenotype prevalence in the Korean population compared to other ethnic populations and its association with RBC alloantibody frequency. Transfus Med 2019;29:415-22. [Crossref] [PubMed]
- Rouger P, Ruffie J, Gueguen A, et al. Human blood groups of the Chinese population of Macau 1. Blood groups ABO, Rhesus, MNSs, Kidd, Duffy and Diego. Journal of Human Evolution 1982;11:481-6. [Crossref]
- Yu Y, Ma C, Sun X, et al. Frequencies of red blood cell major blood group antigens and phenotypes in the Chinese Han population from Mainland China. Int J Immunogenet 2016;43:226-35. [Crossref] [PubMed]
- Hirani R, Weinert N, Irving DO. The distribution of ABO RhD blood groups in Australia, based on blood donor and blood sample pathology data. Med J Aust 2022;216:291-5. [Crossref] [PubMed]
- Liao H, Li J. Distribution characteristics of ABO and RhD blood groups among the voluntary blood donors in Chongqing: A retrospective study. Medicine (Baltimore) 2020;99:e22689. [Crossref] [PubMed]
- Liu J, Zhang S, Wang Q, et al. Frequencies and ethnic distribution of ABO and RhD blood groups in China: a population-based cross-sectional study. BMJ Open 2017;7:e018476. [Crossref] [PubMed]
-
Hong Kong SAR Government Census and Statistics Department 2023 [updated 4/4/2023; cited 2023 3/8/2023] . - Sun CF. The distribution of blood group antigens among Chinese in Taiwan. Transfusion 1989;29:463. [Crossref] [PubMed]
- Lin-Chu M, Broadberry RE, Chang FJ. The distribution of blood group antigens and alloantibodies among Chinese in Taiwan. Transfusion 1988;28:350-2. [Crossref] [PubMed]
- Sun Y, Wang L, Niu J, et al. Distribution characteristics of ABO blood groups in China. Heliyon 2022;8:e10568. [Crossref] [PubMed]
- Reid ME, Lomas-Francis C, Olsson ML. The Blood Group Antigen Facts Book (Third Edition). Boston: Academic Press; 2012.
Cite this article as: Ng YW, Tong CY, Tsoi WC, Lee CK. Frequencies of ABO and RhD blood groups among blood donors in Hong Kong. Ann Blood 2023;8:33.


