
Ptosis and diplopia—sole manifestations in multiple myeloma
Introduction
Multiple myeloma is a plasma cell dyscrasias, associated with the neoplastic proliferation of plasma cells and their precursors. Orbital plasmacytomas are the localised forms, arising in the orbit and comprise 3% of all orbital tumours. Diplopia and ptosis result from interference of mechanical function of the orbital muscles. We present an unusual case of multiple myeloma, where the only initial symptoms were ptosis and diplopia, secondary to mechanical restriction of the ocular muscles (superior rectus and levator palpebrae superioris)
Case presentation
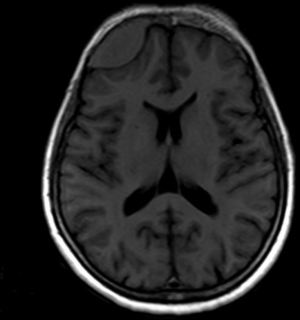
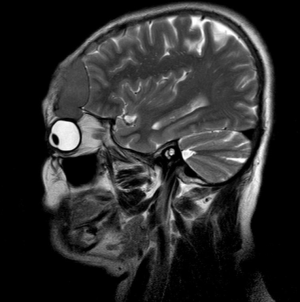
A 63-year-old female, with no significant ophthalmic history presented with drooping of her right eyelid and diplopia of 4 months duration. Examination revealed right upper lid ptosis, normal visual acuity (6/5) in both the eyes, diplopia in all directions of gaze, vertical muscle imbalance and limitation of elevation in the right eye. MRI of the brain demonstrated multiple calvarial lesions with the largest measuring (4.4×2.7×2.8 cm) in the right frontal bone (Figures 1-3). The intra-cranial component of this lesion extended into the extracerebral space, compressed the anterior part of right frontal lobe, extended inferiorly to the right orbital roof, orbital ridge, with intraorbital extension, compressing the superior rectus, levator superioris and indenting the superior margin of the globe.

Haematological investigations revealed normal cell counts with elevated ESR (>140) and biochemical parameters demonstrated reversed albumin/globulin ratio (4.3/4.7 gm). Serum electrophoresis revealed two bands in gamma globulin (possibly dimer and oligomer of IgA). Immune fixation electrophoresis showed two bands in IgA lane and two bands in Kappa lane, confirming the diagnosis of IgA Kappa monoclonal gammopathy. Quantitative estimation of serum immunoglobulins revealed IgA −2471 g/dL and elevated kappa −191.4 g/dL Bone marrow aspiration showed plasmacytosis (12%) and bone marrow biopsy confirmed plasma cell myeloma Patient was diagnosed to have IgA Kappa multiple myeloma ISS stage 1. She was managed with bortezomib, lenalidomide and dexamethasone chemotherapy. She attained very good partial response status and is at present on Lenalidomide maintenance.
Discussion
Plasma cell tumours rarely affect the orbit and they comprise 3% of orbital tumours (1). In multiple myeloma, orbital involvement is a very rare finding. In four series of orbital tumours, incidence of such a presentation varied from 1 in 200 to 1 in 800 (2). Orbital plasmacytomas can be either primary or secondary. Secondary plasmacytomas are ocular manifestations of multiple myeloma and are more common and more aggressive than primary plasmacytoma. Primary and secondary plasmacytomas cannot be differentiated histologically. They can be distinguished clinically with appropriate diagnostic evaluation for systemic disease involvement (3).
Proptosis is the most common manifestation of orbital plasmacytomas (4). Ptosis, diplopia and eyelid swellings are the other common manifestations. Uncommon manifestations include orbital cellulitis (5), fungating eyelid lesions, Tolosa Hunt syndrome (6), orbital hemorrhage (7) and periorbital ecchymosis (8). Though diplopia and ptosis have been documented as manifestations in 23% and 13% of multiple myeloma patients respectively (9), there has been only one case report where these symptoms have been the sole initial manifestations. Multiple myeloma may cause ocular pathology by direct infiltration or as extramedullary plasmacytomas resulting in compression or displacement of tissues, by immunoglobulin light chain deposition in ocular tissues, or by causing hyperviscosity syndrome. In our patient, the ocular manifestations were due to direct infiltration by extramedullary plasmacytomas. A similar case of myeloma presenting with ptosis and diplopia as the sole presenting features due to frontal bone plasmacytoma has been previously reported by Galea et al. (10).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aob.2017.07.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shinder R, Al-Zubidi N, Esmaeli B. Survey of orbital tumors at a comprehensive cancer center in the United States. Head Neck 2011;33:610-4. [Crossref] [PubMed]
- Rodman HI, Font RL. Orbital involvement in multiple myeloma. Review of the literature and report of three cases. Arch Ophthalmol 1972;87:30-5. [Crossref] [PubMed]
- de Smet MD, Rootman J. Orbital manifestations of plasmacytic lymphoproliferations. Ophthalmology 1987;94:995-1003. [Crossref] [PubMed]
- Burkat CN, Van Buren JJ, Lucarelli MJ. Characteristics of orbital multiple myeloma: a case report and literature review. Surv Ophthalmol 2009;54:697-704. [Crossref] [PubMed]
- Kelly SP, Lloyd IC, Anderson H, et al. Solitary extramedullary plasmacytoma of the maxillary antrum and orbit presenting as acute bacterial orbital cellulitis. Br J Ophthalmol 1991;75:438-9. [Crossref] [PubMed]
- Ko S, Huang SY, Liu CY. Extramedullary plasmacytoma masquerading as Tolosa-Hunt syndrome: a case report. BMJ Case Rep 2009;2009. pii: bcr08.2008.0804.
- Almousa R, Shuen C, Sundar G. Acute orbital hemorrhage as a presentation of a lytic bony lesion. Craniomaxillofac Trauma Reconstr 2011;4:189-92. [Crossref] [PubMed]
- Goldstein DA, Schteingart MT, Birnbaum AD, et al. Bilateral eyelid ecchymoses and corneal crystals: an unusual presentation of multiple myeloma. Cornea 2005;24:757-8. [Crossref] [PubMed]
- Swerdlow SH, Campo E, Harris NL, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th edition. WHO Press, 2008.
- Galea M, McMillan N, Weir C. Diplopia and variable ptosis as the sole initial findings in a case of orbital plasmacytoma and multiple myeloma. Semin Ophthalmol 2015;30:235-7. [Crossref] [PubMed]
Cite this article as: Nambiar RK, Nair SG, Mathew SP, Manohar AT. Ptosis and diplopia—sole manifestations in multiple myeloma. Ann Blood 2017;2:9.


