Strategies to meet blood demand for transfusions during the COVID-19 pandemic: lessons learnt from a large central hospital in Malawi
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the cause of coronavirus disease-19 (COVID-19), first detected in Wuhan city, China in December 2019, caused health system-related disruptions. Some data suggest that as many as 50% of cases can be asymptomatic (1). The World Health Organization (WHO) described the novel SARS-CoV-2 outbreak as a “Public Health Emergency of International Concern” on 30th January 2020 and declared it a pandemic on 11th March 2020 (1). The WHO African Region (AFRO) detected its first COVID-19 case in Algeria on the 25th of February 2020 (2). Malawi was declared “a state of disaster” in mid-March 2020 and recorded the first confirmed case on 1st April 2020 (3).
The early days of the COVID-19 outbreak were characterized by lockdowns in many countries following the WHO recommendations, which emphasized the need for restricting large gatherings. The COVID-19 pandemic has affected worldwide blood supplies (4,5). As of May 2020, Morocco was only able to collect 200 blood donations out of its daily target of 800 donations (5). In a survey of WHO Eastern Mediterranean Region (EMR) countries, most blood centers reported that they experienced a decrease in the blood supply during the first month of the pandemic, ranging between 10–75% (5). The respondents attributed this reduction to different factors including decreased in-house collections and cancellations of blood drives due to the closure of universities and institutions, while others believed that public fear of contracting COVID-19 contributed to the decrease in donations. This reduction could be mainly attributed to unintended consequences of stay-at-home orders as well as cancellations of blood drives due to social distancing requirements. In Zhejiang province in China, the number of whole blood donors dropped by 67% and the success rate of recruitment for donations dropped by 60% (6).
A study done by the WHO in the AFRO also documented reduction in blood donations. By June 2020, 3 months into the COVID-19 pandemic, the Malawi Blood Transfusion Service (MBTS) reported a 6% reduction in blood donations in Malawi, and this was before the peak of the first wave, which occurred around mid-July 2020 (7). Few studies have documented how the reduction in blood collection impacts distribution within hospital departments and ultimately healthcare to patients. A study conducted at a teaching hospital in Nigeria revealed that 71.4% of patients with various types of malignancies such as acute myeloid leukemia, bladder cancer, extra-orbital malignancy, prostate cancer, and lung cancer died due to the lockdown imposed in the country, which disrupted the availability of blood donations (8).
This is a mixed-methods study that aims to examine how the COVID-19 pandemic affected blood collection and supply to a major referral hospital in Malawi. Data from administrative records as well as interviews with key informants were conducted. The results identified challenges encountered by the MBTS in blood collection, strategies implemented by the MBTS and Queen Elizabeth Central Hospital (QECH) to mitigate the impact of COVID-19, and recommendations for future pandemics or disasters.
Methods
Settings
The QECH is a public hospital located in Blantyre, the second largest city in Malawi. There are five major departments at QECH: Adult Emergency & Trauma, Obstetrics & Gynecology, Pediatric & Child Health, Medicine, and Surgery. In addition, there are small wards that admit a small number of patients and are categorized as “other” in this report. The hospital serves as a referral location for complex cases. It admits about 65,000 patients, and performs 11,000 blood transfusions annually. It receives its blood supply from the MBTS. The MBTS has four regional centers that are responsible for the collection, processing, production and distribution of blood and blood products to all public and private health facilities.
The MBTS collects blood through in-house donation sessions at regional offices and blood drives campaigns in schools, workplaces, and places of worship. The MBTS collects about 70,000 units of blood annually while the estimated annual national blood need is 120,000 units (9). Under a mandate instituted by the government of Malawi at MBTS’ inception, family member donations are only permitted at hospitals when blood is not available from MBTS.
Data collection
A mixed method study design that utilized both quantitative data and qualitative data was adopted. This was a concurrent triangulation as we collected qualitative and quantitative data at the same time. Data source triangulation was employed to strengthen data validity. Data triangulation is the use of multiple data sources for the purpose of validating conclusions (10). This triangulation design allowed the team to obtain different, but complementary, data about the impact of COVID-19 on blood supplies. The quantitative part of the study was both retrospective and prospective. We prospectively collected data on blood collection and supplies from May 2020 to November 2020. We compared the data with retrospectively collected data from April to November 2019 (pre-COVID), and for April to May 2020.
The quantitative data were extracted from the Blood Donor Management System (BDMS) at the MBTS and the District Health Information Software 2 (DHIS2) at QECH. The data collected includes number of blood drives conducted, number of blood units donated, number of units requested by QECH, number of patients admitted, and number of blood units transfused to patients among the following departments: Adult Emergency & Trauma, Pediatric & Child Health, Obstetrics & Gynecology, Medicine, and Surgery. The data were collected by three research assistants with a minimum qualification of Bachelor of Science in a health-related field and a minimum of 1 year of research experience. Abstracted data were captured onto an Excel spreadsheet, before being exported into STATA 15 (11).
Qualitative data were collected from key informants at QECH, and MBTS. Interviews with purposefully selected clinical staff, nurses, and managers were conducted to explore reasons for trends, to identify useful interventions and transferable lessons. Most of the interviews were completed during the months of July and August 2020, but due to delays caused by the COVID-19 pandemic, few were conducted in December 2020 because participants were not available during the scheduled months. The study adapted a purposive sampling technique to recruit respondents for qualitative data collection.
There were 16 one-to-one interviews completed in total. While there are no fixed rules for sample size in qualitative research, it should be based on information needed and a guiding principle of obtaining data saturation (10). However, some authors have recommended a sample size of at least 12 (12,13). Eligible participants were those who provide clinical service, had worked at the sites for at least 6 months and willing to provide informed consent were included. At the hospital level, respondents primarily came from the wards and the laboratory department. At the MBTS, we interviewed 4 individuals from key departments: 2 laboratory technicians and 2 senior managers in charge of blood collection. On average, each interview lasted for 30–60 minutes and was audio-taped.
The interviews were performed by one research assistant, while two research assistants abstracted data from QECH and MBTS systems. The research assistants underwent a 1-week orientation to familiarize themselves with the data collection tools. The tools were piloted before the actual data collection began.
Data analysis
We compared blood donation activities (in-house and outside blood drives) and number of blood units collected by the MBTS, blood supply and demand at QECH, and blood transfusions among all departments at QECH. We compared monthly data for 8 months during the COVID-19 pandemic with data from the previous year. To have a broader understanding of blood product utilization patterns during this period, we also compared hospital admissions and blood transfusion rates.
For the qualitative data analysis, we used Nvivo software. During the analysis, we thoroughly read the individual interview guides and selected interview scripts from each category to identify the main themes. The themes were assigned codes. The codes were both inductive and deductive. The list of the themes was expanded as additional themes emerged from the interviews.
To ensure data quality, investigators closely reviewed the data on an ongoing basis to ensure full and correct compilation of results and to provide feedback to the research assistants on how to improve procedures of their work. The quality assurance measures included: applying consistency checks to test the internal validity of data fields; ensuring proper documentation during data collection and processing; and ensuring that data was clean and accessible before the analysis.
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was reviewed and approved by the ethics committee of the College of Medicine Research Ethics Committee (COMREC), at the Kamuzu University of Health Sciences (No. P.04/20/3037). The interviewer reviewed a consent form with the participant and consent was obtained prior to beginning each interview. All interviews took place in either a private room or office to maintain confidentiality and were conducted in the language preferred by the participant, either Chichewa or English.
Results
Blood donation activities
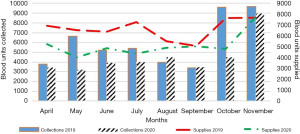
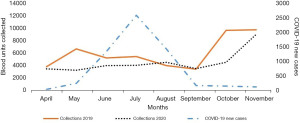
During the first 8 months of the COVID-19 pandemic (April to November 2020), 1,777 blood donation drives were conducted compared with 2,587 drives during the same period in 2019. This translated to 31% reduction in blood collection drives (Table 1). The number of whole blood units collected during the first 8 months of COVID-19 pandemic were 36,150, compared to 47,759 during the same period in 2019. This translates to a 24% reduction in blood collections. However, the difference was not statistically significant (Table 1). As shown in Figure 1, the number of operating blood collection drives was maintained despite the peak in the number of COVID-19 cases (2,573 cases) in mid-July 2020.
Table 1
| Description | 2019 | 2020 | Difference | % | P value |
|---|---|---|---|---|---|
| MBTS | |||||
| Blood collection drives | 2,587 | 1,777 | −810 | −31 | 0.004 |
| Total blood units collected | 47,759 | 36,150 | −11,609 | −24 | 0.20 |
| Total blood and blood products supplied | 53,089 | 41,028 | −1,2061 | −23 | 0.012 |
| QECH | |||||
| Total units requested | 11,079 | 10,210 | −869 | −8 | 0.53 |
| Total units issued | 7,303 | 6,028 | −1,275 | −17 | 0.04 |
*, April to November 2019 and 2020. Negative (−) denotes decline. The data is for 8 months period, during COVID-19 and prior to COVID-19. MBTS, Malawi Blood Transfusion Service; QECH, Queen Elizabeth Central Hospital; COVID-19, coronavirus disease-19.

The was no relationship between number of COVID-19 new cases and number of blood units collected (Figure 2). The blood collections steadily increased from May to August with a reduction in September, then increased from October to November 2020. There were 533 additional units collected in August 2020 (COVID-19 pandemic period) respectively compared to the same month in 2019 (Figure 2), despite the fact that the number of blood collection drives were fewer in 2020 (Figure 1).
The reduction in the number of blood units collected greatly affected the number of units supplied to QECH. All participants in the study agreed that COVID-19 had adversely affected blood availability. Key informants reported that during the study period, QECH experienced shortages of blood and blood products required for transfusion. They attributed the worsened shortage to the inability of the MBTS to collect sufficient number of units from the blood donors due to COVID-19.
This is supported by the responded below:
“I would say that blood was available but it was not enough, as usual we don’t have enough but I think during the peak of COVID-19, it was a bit worse.” (QECH senior laboratory personnel).
This was also corroborated by the responded below:
“At least now because the pandemic things are getting to normal, but then when it was at its peak, it was really a challenge. Even in the high dependency unit (HDU), after requesting blood, we were just been told that we don’t have blood, and you just document on the patient’s file that there is no blood.” (Nursing officer, HDU, maternity, QECH).
Reasons for low blood units’ collections
The reduction in the number of blood units was heavily influenced by the closing of schools. This perspective was reinforced in the response below:
“You know, 75% of our donors are students from secondary schools, and this time around the secondary schools were closed, so we had problems accessing them.” (Senior MBTS personnel).
COVID-19 not only negatively affected blood donation drives but also the availability and willingness of blood donors to present for blood donation. Participants explained that potential blood donors elected not to participate in blood donation drives because of fear of contracting the virus. One COVID-19 preventive measure was to avoid crowded places. Many people believed that blood donation drives could create a fertile ground for COVID-19 transmission if preventive measures were not strictly adhered to. Relatedly, it was difficult for MBTS blood donation teams to organize blood donation drives as public gatherings were banned due to safety concerns.
The fear of contracting COVID-19 was evident in our study as reported below:
“Yes, I would be afraid in general to contract COVID-19, and this now will depend on the passion of the person to donate. No one would want to put his life at risk.” (Clinician, Obstetrics & Gynecology—QECH).
Impact on transfusion services
During the first 8 months of pandemic, there were 41,028 units of blood and blood products supplied to all hospitals in Malawi by the MBTS, which is significantly lower than what has been supplied in 2019 (Table 1). The number of units requested by QECH dropped from 11,079 in 2019 to 10,210 in 2020 (P<0.53, Table 1). Blood supply to QECH dropped by 17% (P<0.04). The number of blood products supplied to all hospitals were lower during the COVID-19 period compared to 2019, with exception of the month of November (Figure 3). This is despite the fact that the number of blood units collected in November 2020 was less than the number of blood units collected in 2019.
Hospital admissions requiring blood transfusions
The admissions in 2020 were lower than 2019 by 9,580 admissions. The differences in number of admissions to various departments were all statistically significant (Table 2). There was a reduction in the number of units transfused across all departments except cases categories under “Other”. The biggest reduction was in the Adult Emergency & Trauma department (29%) while the smallest was noted in Obstetrics & Gynecology and Pediatric & Child Health departments (17% for each). There was an increase in the number of units transfused in “Other” departments (20%), but this did not reach statistical significance (P<0.63) (Table 2).
Table 2
| Description | 2019 | 2020 | Difference | % | P value |
|---|---|---|---|---|---|
| Admissions | |||||
| Adult Emergency & Trauma | 2,131 | 1,764 | −165 | −7 | 0.01 |
| Obstetrics & Gynecology | 22,134 | 19,689 | −2,445 | −11 | 0.006 |
| Pediatric | 12,285 | 9,160 | −3,125 | −25 | 0.0009 |
| Medicine | 6,629 | 5,373 | −1,256 | −20 | 0.001 |
| Surgery | 3,828 | 2,414 | −1,414 | −37 | 0.0003 |
| Other departments | 1,599 | 626 | −973 | −61 | 0.0009 |
| Transfusions | |||||
| Adult Emergency & Trauma | 1,502 | 1,065 | −437 | −29 | 0.007 |
| Obstetrics & Gynecology | 1,754 | 1,455 | −299 | −17 | 0.10 |
| Pediatric & Child Health | 1,699 | 1,407 | −292 | −17 | 0.04 |
| Medicine | 1,341 | 964 | −377 | −28 | 0.004 |
| Surgery | 609 | 472 | −137 | −22 | 0.11 |
| Other departments/wardsꝉ | 381 | 459 | +78 | +20 | 0.63 |
*, April to November 2019 and 2020; ꝉ, Pediatric: Orthopedic, Neurosurgery; Surgical: Burns, ENT, Ophthalmology. QECH, Queen Elizabeth Central Hospital; ENT, Ear, Nose, and Throat.
The lowest reduction reported at Obstetrics & Gynecology and Pediatric departments was reported to be due to prioritization in issuing blood for specific patients. This is supported by the respondent below:
“I think one big challenge is that blood is never enough for every patient so every day we are prioritizing, like which patient to give blood to.” (Laboratory personnel QECH).
Mitigation strategies
The MBTS had devised a strategy on blood collection, as reported below:
“On blood collection, we intensified on village/community blood collection drives whereby we would go there at the trading center, with our loud music equipment and everything, people come and donate, so, those are the strategies which we had to put in place…And we collected, you know, quite a large amount of blood pints so that, of course the COVID-19 pandemic affected us but not as we expected.” (MBTS personnel).
In order to reduce fears of contracting COVID-19 among blood donors and staff, the MBTS put up strategies to reduce COVID-19 transmission as follows:
“Yeah, fears are there because, you know, COVID-19 is asymptomatic. You cannot know that somebody has got COVID-19 but we put in place measures whereby at least we are trying to reduce the spread of COVID-19, we treat our donors as somebody who can have COVID-19... We check temperatures just to make sure that the donor has no fevers, and we have got a questionnaire that we have just developed... If you have been outside the country or you have been in contact with a person with COVID-19, those people we would not allow them to pass through the process... To some extent, we feel safe because it’s like we sieve the donors that we think may have some symptoms like the flu, fever… We don’t allow them to come in...” (MBTS personnel).
Discussion
Our results provide an overview on the impact of the COVID-19 pandemic on blood supplies at a referral hospital in Malawi. The results provide insights into a relatively resilient transfusion service that maintained blood supply during the pandemic and how clinical staff at hospitals mitigated the blood shortage so that patients in need of blood were less affected.
Most of transfusion services in Africa already face chronic blood shortages, the COVID-19 worsened the situation. Similar to other countries in Sub-Saharan Africa, the COVID-19 pandemic has had a negative impact on blood transfusion service and hospitals in Malawi. Closure of schools on 28th March 2020 and restrictions on public gatherings due to the pandemic resulted in 31% reduction in blood collection drives conducted by the MBTS. Very few blood donation drives were held at private companies as these were also closed during the first wave of the pandemic. The reduction in blood supplies calculated at QECH was similar to findings from other countries in Sub-Saharan Africa, including from Zambia (14), South Africa (15), Kenya, Tanzania, and Zimbabwe (7).
It is encouraging to note that the reduction in blood units collected were not significant. This might suggest that the measures implemented by MBTS targeting high yield audiences and venues were effective leading to improved donor mobilization strategies. Since schools were closed during the COVID-19 period, the MBTS targeted the communities by conducting blood donation drives in other avenues. Most blood was collected from village/community blood drives as opposed to the school blood drives. There were also consistent blood donation awareness announcements both on mainstream media and social media.
Although most countries reported decrease in blood collections, Burundi and Ethiopia collected more during the first 5 months of the pandemic compared to the previous years (8). We recommend that the MBTS learn from successful counterparts elsewhere about strategies to maintain blood collection during disruption to the system. Blood collection strategies aimed at maintaining and increasing blood collection during a disruption such as COVID-19 must ensure strict adherence to ethical considerations and not compromise on blood safety. In cases where countries collected more blood than needed through donations during the COVID-19 pandemic, it is possible that people were more altruistic. However, excess supply is also a problem, particularly in LMICs, and transfusion services that meet their annual demand should consider scaling down on blood collection drives during pandemics so as to avoid unnecessary wastage. Furthermore, where legally acceptable, countries should consider sharing the excess blood and blood products collected to minimize wastage.
During the pandemic, the number of patients admitted declined, which likely explains the decrease in blood demand. Although the reduction in number of blood collection drives did not result in statistically significant reduction of blood units collected by the MBTS, number of units transfused to patients in several departments decreased. During COVID-19 pandemic, much of clinical care and attention was diverted to COVID-9 patients that most out-patient clinics were cancelled. This diversion of care likely affected the provision of care for certain group of patients (e.g., sickle cell disease among others), as patients needing regular visits were not able to access the services during the first months of COVID-19.
At QECH, the decline in the number of admissions was least at Adult Emergency & Trauma and Obstetrics & Gynecology departments. We could speculate that despite the admissions to the Accident and Emergency department declined, traumas due to road traffic accidents were probably continued as there was no movement restrictions between the districts. The trend at Obstetrics & Gynecology department was also expected as most pregnant clients continued to seek specialized care at QECH when the need arose. It is therefore recommended that these departments should have all the necessary resources to execute their daily activities in future similar disasters.
We noted that prioritization of blood units to certain group of patients. This potentially would mean that blood units were mainly transfused to patients with bleeding emergencies, e.g., postpartum hemorrhage or pediatric patients with severe anemia due to malaria or sickle cell disease in crisis. This observation is supported by one of the senior laboratory personnel at QECH who mentioned that the blood bank staff were faced with the task of prioritizing patients who needed to get blood first because there are never enough blood units. This could be one of the reasons the Obstetrics & Gynecology and Pediatric departments had the lowest decline in the number of units transfused. Other strategies instituted to mitigate the impact of blood shortage were use of uterotonics, suspension of elective procedures at surgical department and ensuring that hematinic was available for patients with chronic anemia, e.g., patients with underlying sickle cell anemia.
Although mixed methods increase scientific rigor, this study has several limitations. On the quantitative data, both retrospective and prospective data were abstracted from institutional databases, as such selection bias could not be ruled out especially on the retrospective reporting due to missing data. We could not directly document the actual decrease in the number of units transfused to a specific group of patients. Interviews with study participants might be prone to social desirability bias. We advocate for a review of blood use at peripheral district hospitals (some of which are as far as 250 KM away from the national blood distribution centers) to provide broader picture beyond our centers.
Conclusions
In Malawi, the COVID-19 pandemic has led to an overall reduction in blood supply and blood donations. Some mitigating measures such as conducting village blood drives and prioritizing blood to patients in need were implemented and yielded encouraging results in terms of maintaining supply for obstetrics and pediatric use. Specific protocols should be developed for disaster management planning, including guidelines for future pandemics.
Acknowledgments
We would like to thank all stakeholders who shared their valuable insights, the Ministry of Health, the Kamuzu University of Health Sciences, Dr. Samson Mndolo, Hospital Director and entire management and staff of QECH, Dr. Patrick Kamalo and entire members of QECH Research Committee, Mrs. Natasha Nsamala, management and staff of MBTS. We would also like to acknowledge the following for their contributions to the study. John Malinga Benson, Phylos Bonongwe, Luis Gadama, Sylvester Chabunya, Final Lodzani, Isabel Sikwese, Angella Jambo, Misheck Kagalu, Vincent Mgode, Thom Mfune, Servace Sakala, Amos Msopera, Yesaya Nyirenda, Gift Msowoya, Josephine Chimoyo, James Aman, J. Chintsanya, Linda Nyondo Mipando, Wongani Nyondo, Emma Malonda, and the entire team at the Research Support Centre. We would also like to recognize Danielle Charlet for her continuous support throughout the study period.
Funding: This research was funded by United States Agency for International Development (USAID) under a cooperative agreement with USAID’s Health Evaluation and Applied Research Development Project (HEARD) (No. AID-OAA-A-17-00002).
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Arwa Z. Al-Riyami) for the series “Blood Transfusion during the COVID-19 Pandemic” published in Annals of Blood. The article has undergone external peer review.
Data Sharing Statement: Available at https://aob.amegroups.com/article/view/10.21037/aob-21-88/dss
Peer Review File: https://aob.amegroups.com/article/view/10.21037/aob-21-88/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aob.amegroups.com/article/view/10.21037/aob-21-88/coif). The series “Blood Transfusion during the COVID-19 Pandemic” was commissioned by the editorial office without any funding or sponsorship. This research was funded by United States Agency for International Development (USAID) under a cooperative agreement with USAID’s Health Evaluation and Applied Research Development Project (HEARD) (No. AID-OAA-A-17-00002). SEN worked for the Malawi Blood Transfusion Service from 2011 to June 2019 and currently works at Queen Elizabeth Central Hospital reviewing patients with hematological conditions. ES worked for the Queen Elizabeth Central Hospital as Laboratory Manager during the study period. FN works for the Malawi Blood Transfusion Service as the Quality Manager. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was reviewed and approved by the ethics committee of the College of Medicine Research Ethics Committee (COMREC), with approval number P.04/20/3037. Those who took part in the Indepth Interview signed consent forms.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506. [Crossref] [PubMed]
- World Health Organization. COVID-19 WHO African Region: External situation report 17/2020. 2020. Available online: https://apps.who.int/iris/handle/10665/332705 (Accessed August 20, 2021).
- World Health Organization. Malawi: WHO Coronavirus Disease (COVID-19) Dashboard. 2020. [cited 2021 Jul 18]. Available online: https://covid19.who.int/region/afro/country/mw
- Stanworth SJ, New HV, Apelseth TO, et al. Effects of the COVID-19 pandemic on supply and use of blood for transfusion. Lancet Haematol 2020;7:e756-64. [Crossref] [PubMed]
- Al-Riyami AZ, Abdella YE, Badawi MA, et al. The impact of COVID-19 pandemic on blood supplies and transfusion services in Eastern Mediterranean Region. Transfus Clin Biol 2021;28:16-24. [Crossref] [PubMed]
- Wang Y, Han W, Pan L, et al. Impact of COVID-19 on blood centres in Zhejiang province China. Vox Sang 2020;115:502-6. [Crossref] [PubMed]
- Loua A, Kasilo OMJ, Nikiema JB, et al. Impact of the COVID-19 pandemic on blood supply and demand in the WHO African Region. Vox Sang 2021;116:774-84. [Crossref] [PubMed]
- Ugwu AO, Madu AJ, Efobi CC, et al. Pattern of blood donation and characteristics of blood donors in Enugu, Southeast Nigeria. Niger J Clin Pract 2018;21:1438-43. [Crossref] [PubMed]
- Njolomole SE, M'baya B, Ndhlovu D, et al. Post baseline situational analysis of blood safety in Malawi 2015. Report of the 2016 survey. Blantyre: Malawi Blood Transfusion Services, 2017.
- Polit DF, Beck CT. Nursing research: Generating and assessing evidence for nursing practice. 9th ed. Philadelphia: Lippincott Williams & Wilkins, 2012.
- Stata 16 Base Reference Manual. College Station: StataCorp., 2017. Available online: https://www.stata.com/manuals/r.pdf (Accessed June 2020).
- Guest G, Bunce A, Johnson L. How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field Methods 2006;18:59-82.
- Watkins DC. Rapid and rigorous qualitative data analysis: the “RADaR” technique for applied research. Int J Qual Methods 2017;16:1609406917712131.
- Kasanga M, Mudenda S, Gondwe T, et al. Impact of COVID-19 on blood donation and transfusion services at Lusaka provincial blood transfusion centre, Zambia. Pan Afr Med J 2020;35:74. [Crossref] [PubMed]
- Kaserer A, Rössler J, Braun J, et al. Impact of a Patient Blood Management monitoring and feedback programme on allogeneic blood transfusions and related costs. Anaesthesia 2019;74:1534-41. [Crossref] [PubMed]
Cite this article as: Njolomole SE, M’baya B, Mandere G, Storey E, Jenny A, Chiwindo T, Nyangu F, Walker D, Muula AS. Strategies to meet blood demand for transfusions during the COVID-19 pandemic: lessons learnt from a large central hospital in Malawi. Ann Blood 2023;8:12.